Custom Telemedicine Apps
In healthcare IT and mobile development since 2005, ScienceSoft designs and develops user-centric telemedicine apps that are loved by patients and physicians.
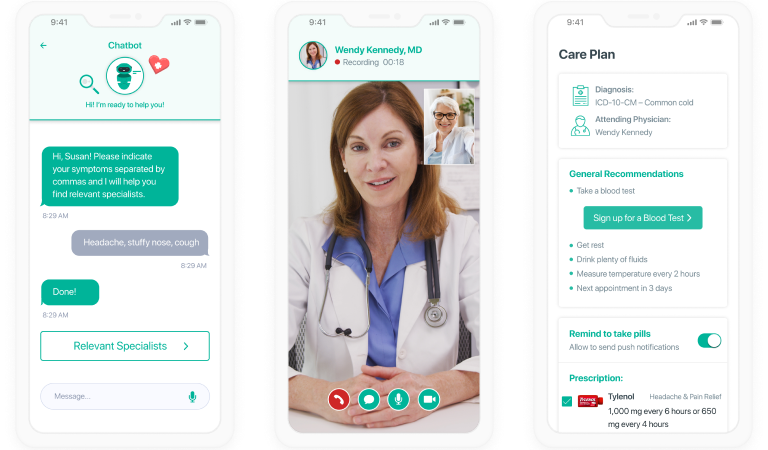
Telehealth apps are used to provide remote healthcare delivery via video calls, messages, file exchange, and vitals tracking. With 150+ healthcare IT projects, ScienceSoft builds SaaS telemedicine products and develops custom telehealth apps for hospitals, practices, nursing homes, and more. Custom telemedicine apps offer features tailored to specific medical specialties, SaMD functionality, seamless integration with existing healthcare systems, and compliance not only with global but also with local regulations.
Types of Telemedicine Apps We Deliver
To help treat patients with conditions like diabetes, COPD, cardiovascular diseases, etc., a telehealth app features:
- Regular online check-ups using audiovisual communication.
- Remote patient monitoring with connected medical devices (e.g., glucose meter, ECG patch) or biosensors measuring vitals.
- Health log with symptoms and vitals.
- Patients’ health data analytics to identify vitals abnormalities, early symptoms of complications, etc.
- Notifications on medications (for patients), alerts on detected abnormalities or risks of complications.
Primary care telehealth apps allow doctors to:
- Conduct virtual first-time appointments.
- Plan the treatment of uncomplicated cases (e.g., mild colds, allergies without complications, indigestion), prescribe medications, and monitor a patient’s progress.
- Schedule screenings, analyses, consultations with other specialists for a wellness exam and conduct follow-ups on the results.
Telehealth apps for providing acute care (e.g., for stroke care in remote/understaffed hospitals) include the following functionality:
- Videoconferencing for emergency consultations.
- Clear UX and intuitive user journeys for doctors.
- Smooth integrations with relevant software (EHR, LIS, RIS, etc.) for streamlined data access.
- Advanced diagnostics features (e.g., AI-driven medical image analysis, VR-based surgery planning).
Telehealth apps are used for nursing care delivery in:
- Preoperative and postoperative patient care.
- Chronic disease management.
- Home care for elderly people.
- Pregnancy monitoring and newborn care.
- Mental health care.
DTx solutions utilize telehealth technologies to:
- Prevent diseases (e.g., apps for patients with prediabetes, atrial fibrillation).
- Help manage diseases and their symptoms (e.g., deliver attention improving therapy for patients with Alzheimer’s syndrome, monitor asthma triggers).
PT and rehabilitation telehealth apps aim at:
- Rehabilitation of motor and cognitive functions after injuries and surgeries.
- Treating chronic orthopedic and neurological conditions (e.g., arthritis, Parkinson’s syndrome).
- Delivering remote physical therapy for athletes.
Teleneurology apps help:
- Monitor and guide patients with chronic neurological diseases (e.g., multiple sclerosis, Tourette syndrome).
- Monitor and manage the recovery process of patients with neurological injuries.
- Provide emergency care departments with online neurological consultations on the treatment of acute conditions (e.g., ischemic stroke).
Telemental app features:
- One-on-one or group online behavioral therapy sessions.
- Patient mental condition assessment.
- 24/7 patient-doctor chat.
- Online chats for peer support groups for patients.
- Prescription renewal/refilling and medication intake monitoring.
We create solutions for:
- Pediatric care delivery to children with chronic conditions or requiring primary care.
- Inpatient care teleconsultations between an on-site pediatrician and a remote pediatric specialist.
- Outpatient pediatric care teleconsultations (e.g., for pediatric dermatology).
- Pediatric care delivery to child care centers, preschools, schools, group homes, summer camps, and juvenile detention centers.
Rural telehealth software allows patients to:
- Request emergency care online.
- Remote access to all major medical services, e.g., primary and specialty care, chronic disease management, mental health services.
- Access a medication plan and renew prescriptions.
- Visit online rehabilitation sessions.
- Monitor health via tracking vitals and symptoms, logging medication intake, etc.
Telestroke software we develop may feature:
- 24/7 audiovisual consultations with a vascular neurologist for remote emergency care teams.
- Integration with EHR, LIS, etc., for streamlined access to patient health data.
- Advanced stroke diagnostics and treatment assistance (e.g., t-PA dose calculator, AI-based CT scans analytics).
- Patient rehabilitation module.
How to Develop a Telemedicine App
The development process of a custom telemedicine app involves several key steps:
1
Requirements gathering and feature set definition
Analyzing the target audience and specific requirements for a telemedicine app to outline its features (e.g., audio/video consultations, appointment scheduling, secure in-app messaging, prescription and refill management), user roles, and integrations.
2
Architecture and tech stack design
Determining the optimal architecture, considering factors like scalability, security, and ease of maintenance; choosing the appropriate technologies for database management, front-end, and back-end development.
3
Project planning
Deciding on the project scope, timeline, deliverables, and resource allocation.
4
Iterative development
Creating the app's user and server side components according to the defined architecture and feature set; integrating the app with other systems (e.g., EHR/EMR, payment gateways) and smart medical devices (e.g., interactive stethoscopes, wearable ECG and glucose monitors).
5
Testing
Detecting and fixing any functional, performance, or security issues; performing unit testing, integration testing, and user acceptance testing to guarantee a stable and reliable platform; ensuring the app’s adherence to healthcare regulatory standards, such as HIPAA, HITECH, and GDPR.
6
Deployment
Configuring the necessary infrastructure, i.e., servers, cloud services, and databases; deploying the app to the desired platform, e.g., iOS, Android, or web.
7
Maintenance
Continuously monitoring and maintaining the app to ensure its high performance and stability; performing regular updates, security patches, and bug fixes; providing ongoing user support and addressing any emerging issues or requests.
Why Choose ScienceSoft?
- 34 years in the IT market.
- 18 years in the healthcare IT industry.
- ISO 13485-certified to design and develop medical software according to the requirements of the FDA and the Council of the European Union.
- Rich experience in developing HIPAA-compliant software.
- Working experience with healthcare standards (e.g., HL7, ICD-10, CPT, XDS/XDS-I).
- UX and UI design aimed at convenience for patients and medical staff.
- ScienceSoft is a 3-Year Champion in The Americas’ Fastest-Growing Companies Rating by the Financial Times.
- Experience with the standards of National Council for Prescription Drug Programs (NCPDP) concerning electronic information exchange (e.g., NCPDP D.0).
- ScienceSoft’s RPM solution won the Best Healthcare Technology Solution Award 2022 from Health Tech Digital.
- ScienceSoft became a finalist for the Health Tech Award 2022 with its laboratory diagnostics software and the HTN Now Awards 2023 in the Excellence in Remote Patient Monitoring category.
ScienceSoft Is a Leader in Healthcare IT Services Market in 2022 SPARK Matrix
ScienceSoft is featured as a leading healthcare IT services provider, along with Athena Health and Oracle Cerner. This achievement is a result of 18 years of tireless pursuit of technological innovation, made possible by ScienceSoft’s passionate team of healthcare IT experts who always strive to make a difference for patients and caregivers alike.
Our Selected Telemedicine and Mobile Health Projects
FAQ about Telemedicine App Development
What are the benefits of cooperating with a vendor on telehealth app development?
In cooperation with ScienceSoft, you will get access to healthcare IT competencies, including mobile and web app development, connected medical devices, chatbots, speech recognition, etc.
Will a telemedicine app be HIPAA-compliant?
If you opt for a platform-based telemedicine app, we test it for HIPAA compliance and deliver a report containing measures taken by a vendor to ensure the safety of PHI.
If you choose to develop a custom telemedicine app, we ensure it is HIPAA-compliant by employing necessary data security measures (data encryption, data anonymization, data access control measures, etc.).
Will a telehealth app work in sync with other internal software systems?
We guarantee seamless integration of a telemedicine app with your internal applications, including EHR/EMR, HIS (hospital information system), and LIS (laboratory information system).
How much does a telehealth app cost?
On average, the costs of a telehealth app range from $150,000 to $400,000 depending on the functional scope and other factors. You are welcome to use our free cost calculator to get a precise estimate for your project.
Choose Your Service Option
Platform-based telemed app implementation consulting
We help you:
- Choose a HIPAA-compliant platform-based telehealth app suitable for your needs.
- Configure and customize the app.
- Test the app.
Custom telemed app development and support
We provide end-to-end telemed development services:
- Business analysis.
- App architecture design.
- App development planning, execution, and management.
- QA and testing planning (incl. test automation, if feasible), execution, and management.
- Integration with existing software.
- User training.
- After-launch support (2-3 months).
Telemedicine app support and evolution
We offer:
- Continuous L1, L2, L3 support.
- Telehealth app maintenance, troubleshooting, proactive monitoring of security and compliance.
- Patient app evolution planning and implementation (new functionality introduction, security measures implementation, UX redesign, etc.)
ScienceSoft USA Corporation Is a 3-Year Champion in the Financial Times Rating
Three years in a row (2022–2024), the Financial Times has included ScienceSoft USA Corporation in the list of 500 fastest-growing American companies. This is the result of our dedication to driving project success despite any constraints and disruptions.

Ready for Your New Telemedicine App?
Virtual care visits are predicted to reach 1 billion by the end of the year. Get your telehealth app now to keep up with the demand.

 Schedule a call
Schedule a call