Telehealth Technology in Healthcare
In healthcare software consulting and development since 2005, ScienceSoft designs and develops various types of telemedicine software for healthcare organizations and software product companies.
Telehealth in Brief
Telehealth technology enables audiovisual patient-doctor communication, patient monitoring, and remote care delivery across healthcare domains. Telemedicine solutions reduce healthcare costs by eliminating the need for in-person visits, increase care accessibility, and automate routine tasks.
Telehealth Market Overview
The global telehealth market is projected to grow from $120.4 billion in 2023 to $285.7 billion by 2028 at a CAGR of 23.2%. According to the MarketsandMarkets, the key drivers of telehealth software adoption are:
- Growing geriatric population.
- Lack of healthcare professionals (especially in rural areas).
- Rising prevalence of chronic conditions.
- Advancements in telecommunication technologies.
Adoption of Telehealth in Healthcare
As of 2024, 78.6% of US hospitals have installed a telemedicine solution. And, according to Rock Health, 63% of US adults surveyed in 2023 have used virtual care at least once within the last 12 months. The primary reasons for choosing telemedicine include convenience and shorter wait time.
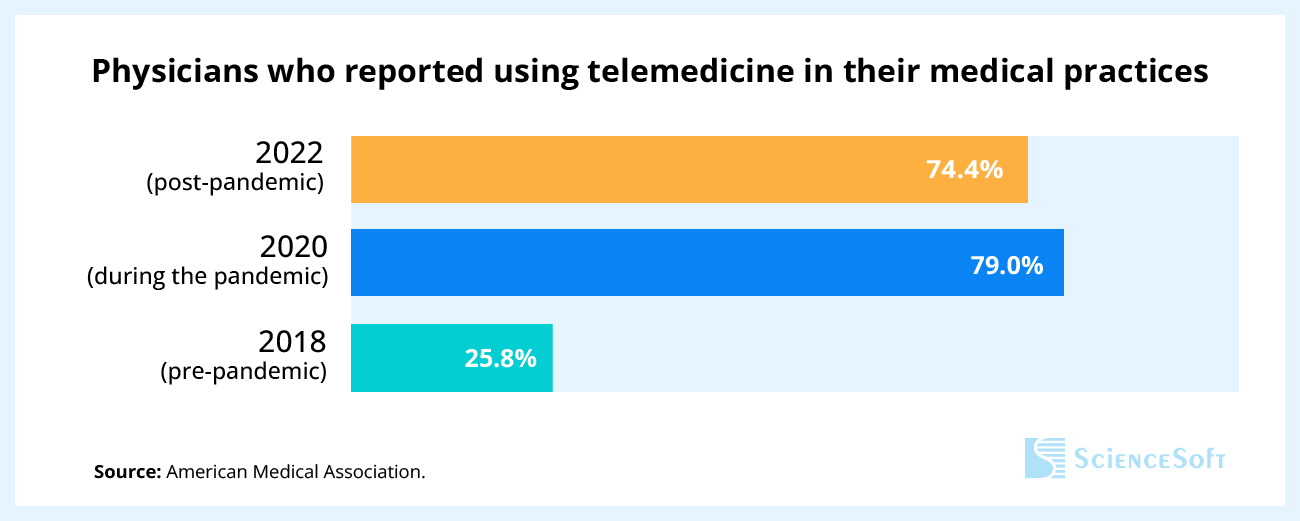
However, since the primary reason for the telemedicine boom was the COVID-19 outbreak, telemedicine usage has decreased after the pandemic.
Is telehealth falling off?
While we see a slight decline in telehealth usage since 2020, the overall adoption level is still several times higher than in pre-pandemic 2018, and we expect it to stay above 70% going forward. After getting familiarized with virtual care in 2020-2021, patients are more willing to continue using it for the sake of convenience and shorter wait times, especially for prescription refills, minor illnesses, or chronic condition management. Healthcare providers also continue to rely on telemedicine to improve care accessibility, streamline clinical workflows, and reduce costs.
The key drivers of telehealth software adoption:
- Increased patient flow and the need to avoid personal contact due to the COVID-19 pandemic.
- Growing demand for care digitalization.
- Alleviated CMS (the Centers for Medicare and Medicaid Services) restrictions for telehealth reimbursements.
- Focus on value-based care and increased care quality.
- Lack of healthcare professionals (especially in rural areas).
Applications of Telehealth Technology
Via synchronous and asynchronous communication, telehealth software enables remote consultations with primary care physicians, ob-gyns, pediatricians, geriatricians, mental health specialists, etc. Also, the impact of telemedicine software for primary care is vital during the COVID-19 pandemic as telehealth minimizes contact between a person infected with a contagious disease and a healthcare specialist.
How primary care telehealth works: After downloading a healthcare provider’s primary care telemedicine app, a patient can choose a doctor, plan an online appointment or request an urgent appointment, sign up for lab tests, screenings, get a prescription renewal, etc. The doctor receives a notification on an initial appointment request, approves it, and sends a pre-visit survey to the patient. During a video appointment, the doctor can study the patient’s medical history, lab tests, and current medications to diagnose the patient and plan treatment in the app.
Use cases:
- First-time consultations on mild cases of common diseases.
- Follow-up consultations with a primary care physician (e.g., to monitor recovery after the flu).
- General consultations with a practitioner on family planning, mental health, regular health check-up results, etc.
The medical staff uses telehealth technology to consult with highly experienced acute and intensive care specialists. This application of telehealth allows delivering quality care to emergency room patients regardless of their location and enhances the expertise of ER staff.
How acute care telehealth works: After receiving an acute care consultation request, a remote acute care specialist initiates a telehealth call with an on-site acute care team to assess a patient, analyze their medical history, lab tests, and medical images, and make a diagnosis. Based on the diagnosis, the acute care consultant helps the on-site team to plan treatment. The doctor can also coordinate care delivery (e.g., surgery) in real time thanks to access to real-time patient data, video monitoring of the patient, and audio communication with the on-site care team.
Specifics of the acute care software architecture: Instead of an app for patients, the solution features an app for the on-site acute care team. The application for the medical staff is used by remote acute care consultants.
Use cases:
- Psychiatric emergencies (e.g., acute excitement with psychomotor agitation, self-destructive or suicidal behavior).
- Major trauma treatment (e.g., after a car accident).
- Stroke treatment assistance.
- Tele-ICU patient monitoring by a remote intensivist.
- Remote supervision by expert surgeons for less experienced doctors providing acute care (e.g., for teaching hospitals).
Telehealth software provides a full scope of healthcare services for rural residents (e.g., primary, acute, specialty care, chronic disease management), improves rural patients' health monitoring, and reduces avoidable travels to a healthcare provider’s office.
How telehealth for rural patients works: Rural residents download their healthcare providers’ telehealth application and use it to schedule online appointments with doctors, ask for prescription refills, browse through educational materials on health topics, conduct self-monitoring of chronic diseases, request emergency care, and more. Doctors or nurses can initiate an online chat with their rural patients to check their recovery, medication side effects, etc. Doctors who treat patients with chronic diseases may receive alerts on troubling symptoms of their patients, or regularly review patient dashboards with patient condition trends.
Use cases:
- Primary care services for rural residents.
- Management of chronic diseases (e.g., diabetes, COPD).
- Remote monitoring for patients with chronic diseases.
- Rural population health monitoring and management.
- Home rehabilitation for rural patients.
Telehealth-enabled virtual hospital
Using virtual hospital software, the medical staff can track patient conditions remotely and provide treatment to patients with chronic diseases who were hospitalized multiple times within 12 months or patients with mild cases of communicable diseases. Such software allows patients to stay in comfortable home settings while getting hospital-level treatment and monitoring.
How telehealth-enabled virtual hospital works: The patients of a virtual hospital have regular telehealth-enabled consultations with required doctors via an app (it can be installed on a personal device like a laptop or on a tablet temporarily provided by the hospital). The doctors can see analyzed patient information from smart connected medical devices (e.g., blood glucose monitors) or sensors (e.g., ECG patches) and can coordinate further treatment accordingly.
Use cases:
- Remote health monitoring of patients with multiple chronic diseases (often geriatric patients).
- Tracking of a patient’s vitals and medication scheme adherence.
- Remote patient care coordination between different healthcare specialists (e.g., a neurologist and a cardiologist).
Telenursing solutions enable remote nursing care delivery and patient monitoring, automated tracking of patient vitals and symptoms, and reduce nurse travel time.
How telenursing works: Nurses use telehealth applications to track patients’ vitals via connected medical devices, use video and audio communication to guide patients through pre-surgical preparation, monitor their recovery, advise on symptom alleviation, track adherence to the care plan, coordinate home care, and ensure timely adjustments to the treatment plan.
Use cases:
- Preoperative and postoperative patient care.
- Chronic disease management to enhance adherence to the care plan, help manage symptoms, and control patients’ health parameters.
- Home care for elderly patients and patients with disabilities.
- Pregnancy monitoring and newborn care.
- Nursing care for mental health patients.
Telemedicine software helps deliver remote care to children of different age groups at their homes, preschools, schools, etc. Thanks to telehealth technology, children can get care in a comfortable environment and are more active and open during virtual consultations compared to the ones in the hospital.
How telehealth pediatrics works: Using a telepediatrics application, a child’s caregiver can plan and hold appointments with a pediatrician for primary care, follow-ups, regular check-ups, and therapy sessions. Depending on the children’s age, the caregivers can engage them in symptoms and vitals logging, self-education on health topics via interactive games or articles in the app. The pediatricians use the app to hold online examinations and appointments with the patients and their caregivers, track patients’ progress and recovery, and adjust the treatment accordingly.
Use cases:
- Primary care and follow-up appointments for children (accompanied by their caregivers).
- Monitoring of pediatric patients with chronic diseases (e.g., asthma, diabetes type 1, heart conditions, ADHD).
- Outpatient pediatric care teleconsultations (e.g., for pediatric dermatology).
- Group and individual physical or behavioral therapy sessions for children.
Neurologists leverage videoconferencing, remote monitoring, patient-doctor communication features of telehealth applications to provide continuous specialized care to the patients with neurological diseases, monitor their state, and share best practices and expertise with a neurological community (e.g., within one hospital chain).
How telehealth for neurology works: With a teleneurology application, a doctor can conduct regular patient check-ups, access insights on patient condition based on symptoms and vitals log analysis, adjust medications and medication dosages, and provide a patient with tools for disease self-management (e.g., guides to mitigate tremor and disrupted sleep, diet recommendations). For a patient with a neurological disease, the app helps get a doctor’s opinion on new disease symptoms, medication side effects, etc. on demand via text messaging, track symptoms, moods and vitals in the app, and have online appointments from the comfort of their homes.
Specifics of the teleneurology software architecture: If the software is designed to be used for remote neurological consultations, it should also feature an application for remote medical specialists from partnering hospitals who require assistance.
Use cases:
- Management of chronic neurological diseases (e.g., epilepsy, multiple sclerosis).
- Remote monitoring and rehabilitation for patients recovering from neurological injuries (e.g., brain injury).
- Remote neurological consultations and assistance for emergency care teams treating acute neurological conditions.
Telehealth for physical therapy
Designed to provide physical therapy remotely, these telehealth applications help physical therapists manage chronic conditions (especially neurological) and enable patient rehabilitation after surgeries and injuries (including sports injuries).
How telehealth for physical therapy works: A physical therapist assigns personalized physical therapy plans with guided and pre-recorded therapy sessions to patients and monitors patient progress and therapy adherence by checking sessions recordings or smart devices data. The physical therapist can adjust therapy plans and schedule follow-up video appointments with patients. Patients can join online physical therapy in the app (it can be held individually or in groups), monitor personal progress, log health parameters after the therapy session, and more.
Use cases:
- Regular physical therapy for geriatric patients (e.g., with multiple sclerosis, Parkinson’s disease).
- Physical therapy for pediatric patients with movement disorders (e.g., cerebral palsy).
- Joints motion restoration and muscle dystrophy treatment after injuries (e.g., spinal cord injury, bone fracture).
- Muscular tissue and strength restoration after surgeries.
Telemental software enables healthcare providers to improve accessibility and quality of care, helps decrease psychological distress for patients compared with in-person visits, increases patient confidentiality, and offers patients a wider selection of mental health specialists.
How telehealth for mental health works: Using a mental health telemedicine app, mental health professionals hold behavioral therapy sessions for their patients, carry out patient condition assessment or group therapies via videoconferencing. Patients can log their medication intake and recent symptoms in the app, and this data can be monitored by mental health specialists.
Use cases:
- One-time consultations and regular appointments with a mental health specialist (e.g., for behavioral therapy).
- Online monitoring of medication intake.
- Monitoring of people with chronic psychological conditions like autism spectrum disorders, anxiety disorders, etc.
- Group therapy and support groups (e.g., for people with alcohol/ drug addiction, people facing the loss of a beloved one).
This type of telehealth software focuses on sharing specialized stroke treatment expertise between a neurological center and several remote emergency care hospitals by leveraging audiovisual communication and remote patient monitoring technologies.
How telehealth for stroke care works: An on-site emergency care team in one of the hospitals reports a new case in telestroke software. A stroke center administrator processes the request and redirects it to an on-duty vascular neurologist who contacts the emergency care team to provide a video consultation, online patient assessment, diagnosis, and a stroke treatment plan.
Specifics of the stroke care software architecture: The solution should include an app for neurological center experts and an app for the on-site stroke care team.
Use cases:
- Stroke type and severity diagnostics.
- Ischemic stroke treatment planning.
- Stroke rehabilitation planning and remote rehabilitation monitoring via smart connected medical devices or sensors to facilitate recovery and decrease the risk of complications (e.g., thrombosis, limb contractures, bedsores).
- Remote stroke care training for emergency care teams.
- Remote supervision by an expert vascular neurologist for doctors providing acute stroke care.
The Architecture of Telemedicine Software
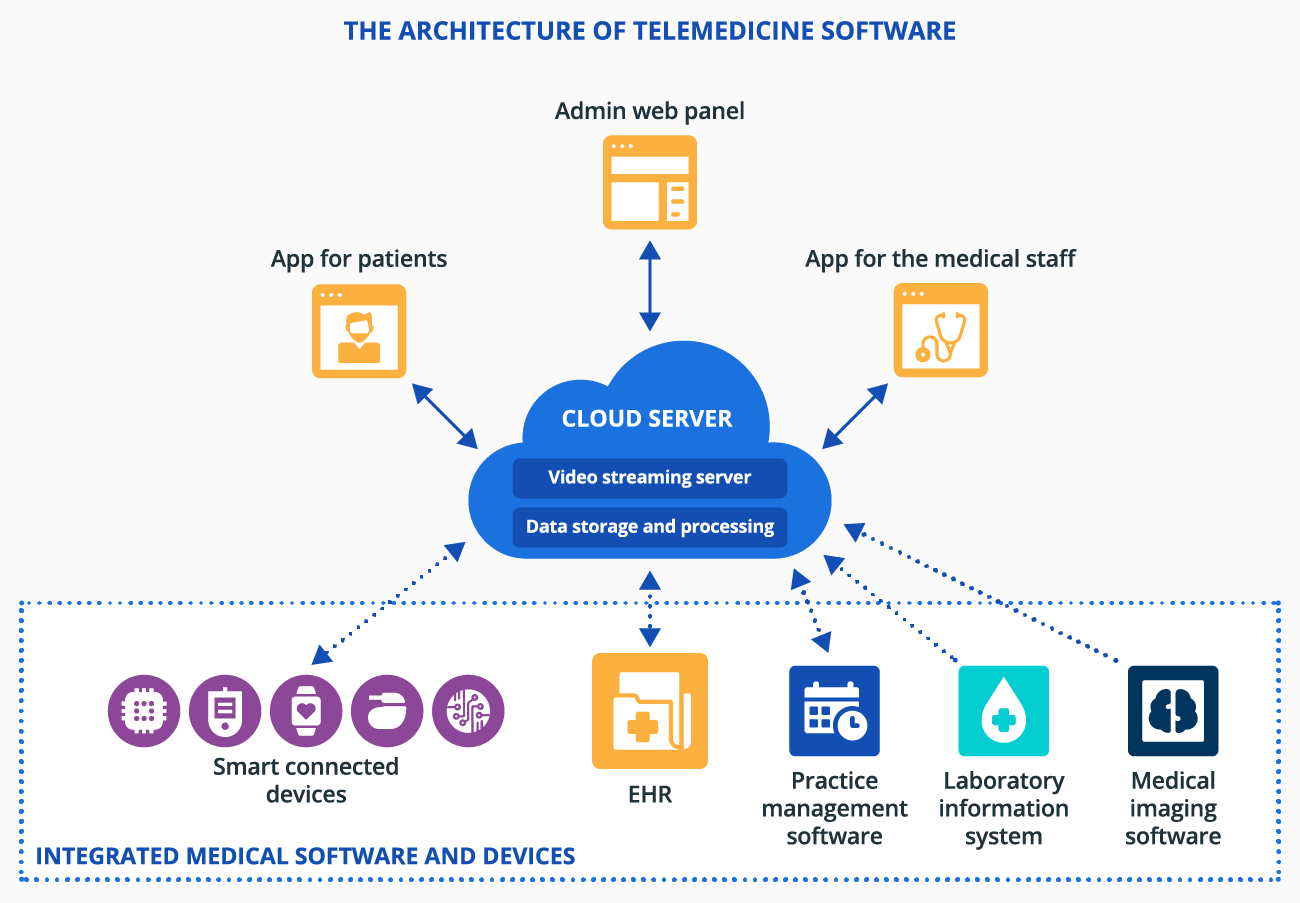
At the core of telemedicine software is a cloud server with modules for video streaming and data storage and processing. Apps for patients and the medical staff communicate with the server to enable video consultations, messaging, and user access to treatment and health information. An admin web panel provides supervisors, hospital administrators, etc., with an interface to grant app access to patients and the medical staff, view and configure a patient list and doctors’ schedules, and more.
Telemedicine software can be integrated with sensors or smart connected medical devices (e.g., smart glucose monitors) to provide remote patient monitoring. Integration with medical software like a laboratory information system, EHR, practice management software, and medical imaging software enables smooth access to patient data for diagnosing, health condition tracking, and more.
Telehealth Consulting and Development by ScienceSoft
ScienceSoft leverages its extensive experience in healthcare software development to design and build telehealth software for virtual care delivery. You set goals, we drive the project to fulfill them in spite of time and budget constraints, as well as changing requirements.
Telehealth adoption consulting
What we do:
- Analyze your needs and elicit requirements for telehealth software.
- Create a detailed specification of telehealth software with a focus on its target use, outline the functionality set.
- Design a high-level architecture, plan required integrations (with EHR, CRM, practice management software, etc.).
- Identify appropriate standards for data exchange (e.g., FHIR, USCDI, NCPDP SCRIPT) and correct handling of structured PHI (e.g., ICD-10, LOINC, SNOMED CT, RxNorm).
- Calculate telehealth software cost, ROI, total cost of ownership, and plan software implementation timelines.
- Provide a regulatory compliance plan (for HIPAA, GDPR, Cures Act, and other relevant regulations).
Development of telehealth software
What we do:
- Analyze your needs and create a telehealth software concept.
- Draw up a comprehensive feature list of your general or specialized telehealth software.
- Plan telehealth software architecture with a focus on flexibility and scalability.
- Develop and test a telehealth software MVP with high-priority features within 4-8 months and roll out the secondary functionality upon the agreed schedule.
- Help comply with required regulations (HIPAA, GDPR, Cures Act, etc.).
- Provide extensive user and admin guides for telehealth software to ensure smooth adoption.
- Support and maintain telehealth software (if required).
About ScienceSoft
In healthcare IT since 2005, ScienceSoft is an international IT consulting and software development company headquartered in McKinney, Texas, US. Being ISO 13485, ISO 27001, ISO 9001 certified, we help healthcare organizations and software product companies design and develop various types of secure telemedicine software relying on a mature quality management system and ensuring the safety of our clients’ data.






