How Healthcare Providers Benefit From EHR-CRM Integration
First with the coming of Meaningful Use and now Value-Based Care to replace it, healthcare providers have been heavily encouraged to adopt IT systems in their practice. For the hospitals and large practices that did adopt electronic health records (EHR), it should be heart-wrenching to think of yet another IT system, considering how time-consuming and expensive such a venture can be. Still, no EHR can satisfy all the needs when it comes to managing relationships with patients.
Now that the industry agenda is all about value, a patient’s quality of life becomes central in this equation that makes up providers’ revenues. The more informed and satisfied a patient is, the less chances there are for healthcare providers to face penalties that cut into their profits. This is where a properly tuned CRM system is a must, as it effectively fills the gaps that can severely affect treatment outcomes.
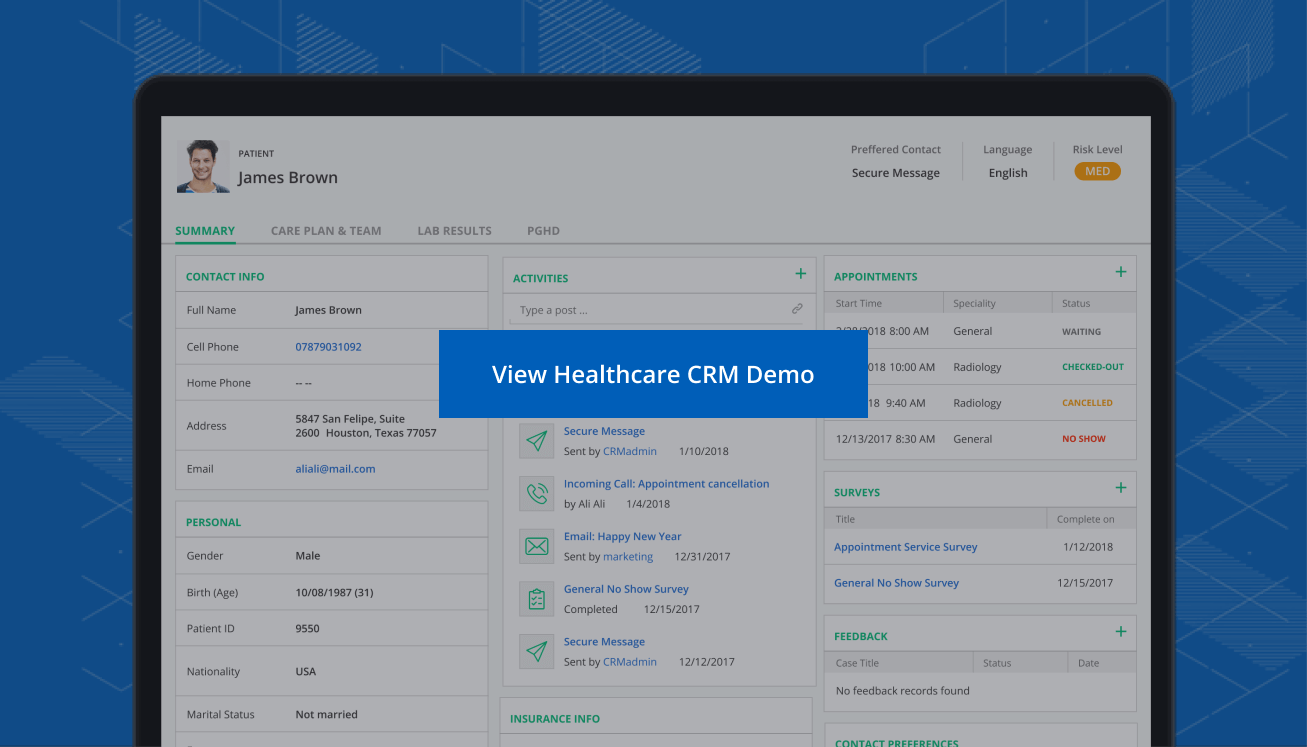
As a system that tracks interactions with patients across every possible channel (both online and offline), it provides a complete picture of a relationship, not necessarily treatment only, which can always be improved or tweaked as required. However, healthcare CRM as such is only making its way to win users. A low awareness of its impressive functional scope and of its direct link to acquiring more patients and delivering higher-quality care is one of the reasons for its moderate adoption rates.
We came up with the overview below to do justice to the system and identify multiple areas where it can effectively complement a more familiar EHR to the benefit of both patients and medical professionals.
How the integration will work
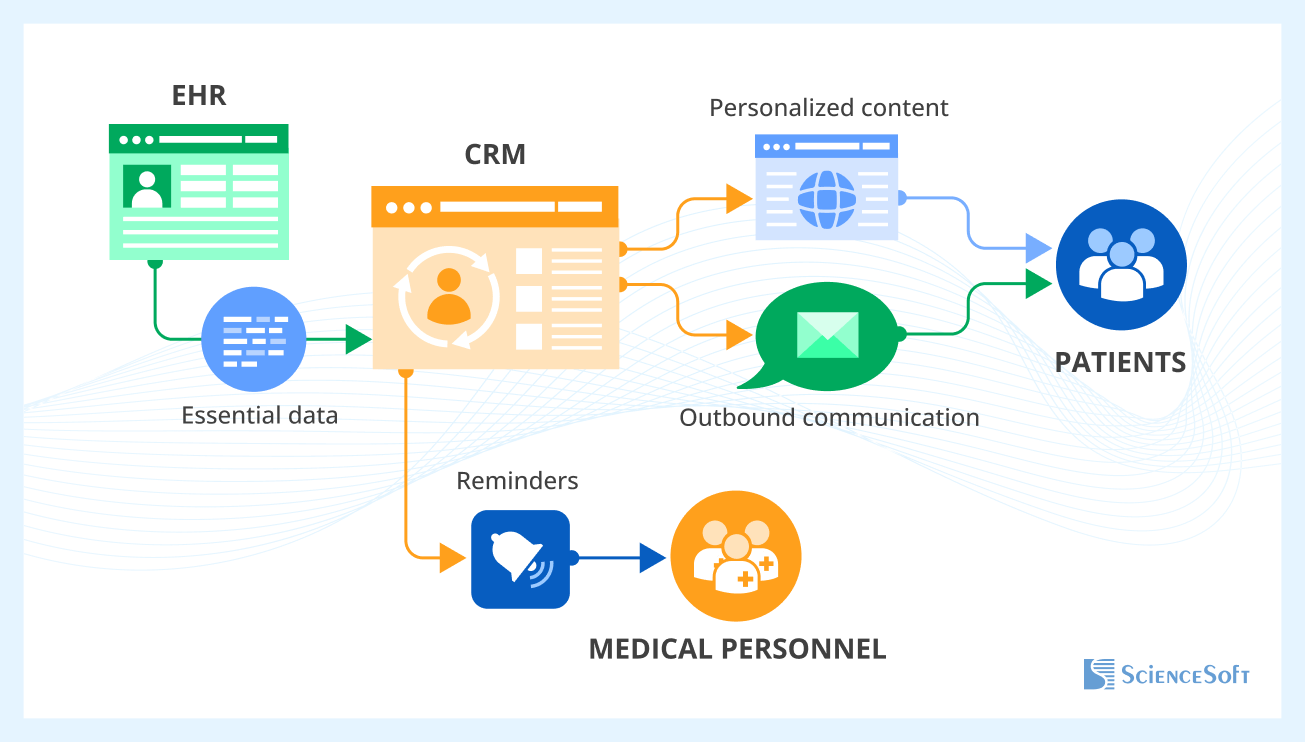
CRM for healthcare can’t function in a vacuum. For truly integrated care, the system has to communicate with other IT solutions adopted at an organization, especially the EHR. The first step here is choosing the communication standard (typically HL7 or FHIR) to ensure data can safely and accurately flow between systems. This step also includes developing a data management strategy: defining the initial data storage format and establishing the data transformation process that will standardize and transfer information across systems.
Depending on the existing IT infrastructure and software, the integration approach can vary. Some organizations go for API-based integration, where the CRM communicates with the EHR directly through exposed endpoints. Others opt for mediated integration, using middleware to manage the data choreography between systems. In setups with multiple applications exchanging data, a common data storage model may be adopted. It will collect and synchronize data from both EHR and CRM into a single, unified database.
Once integration mechanics are chosen, tech teams often have to re-engineer parts of the system architecture, especially if the EHR’s tech stack doesn’t play nicely with the CRM. Here, selecting the right integration tech stack is critical — not only for performance and scalability but also to ensure the resulting system remains HIPAA-compliant and secure.
Once deployed, a correctly integrated CRM will skim the essential data stored in the EHR and feed it to either a patient via email and personalized website content or a care provider to optimize the care delivery process. By identifying website visitors as registered patients, a CRM can trigger medical website personalization and thus encourage patients’ higher conversion and retention rates through serving targeted materials such as relevant new services, follow-up advice on a patient’s recent checks, and more, all in HIPAA-compliant mode.
More functional goals behind such an integration would be to enable (a) outbound communication with patients and (b) notifications and alerts to the personnel. Sounds trivial, but if you look closer, this will take many administrative burdens off care providers’ shoulders and prevent certain communication gaps in doctor-patient relationships that can affect patient satisfaction and loyalty.
How patients and medical staff can benefit from EHR-CRM integration
| Benefit | Impact on healthcare providers | Impact on patients |
| Improved care coordination | Reduced duplication of records | Smoother transitions between care stages |
| Better patient engagement | Automated notifications & follow-ups | Personalized care & reminders |
| Operational efficiency | Less paperwork & manual tasks | Faster response times |
| Enhanced analytics & insights | Patient trends & behavior tracking | Proactive health management |
CRM and pre-care communication
Treatment of chronic or other conditions that don’t require emergency interventions starts with a pre-care stage that only leads up to patient conversion, and it is as much about the right communication as it is about providers’ track record and price.
A healthcare CRM would register every instance of pre-care interactions per prospective patient, through consultations and examinations, to keep up uninterrupted, systematic records. This information could be then used to alert the relevant medical personnel to alarming gaps in scheduled visits (what if they lost a client to competitors) or to notify them about a prospective patient’s intention to resume cooperation in a given period of time.
CRM and interrupted care
For conditions that imply multiple interventions in the long run (e.g., examining the endocrine profile of a woman who is considering pregnancy), keeping up with such patients and guiding them through all the stages is crucial for preventing health deterioration or setbacks.
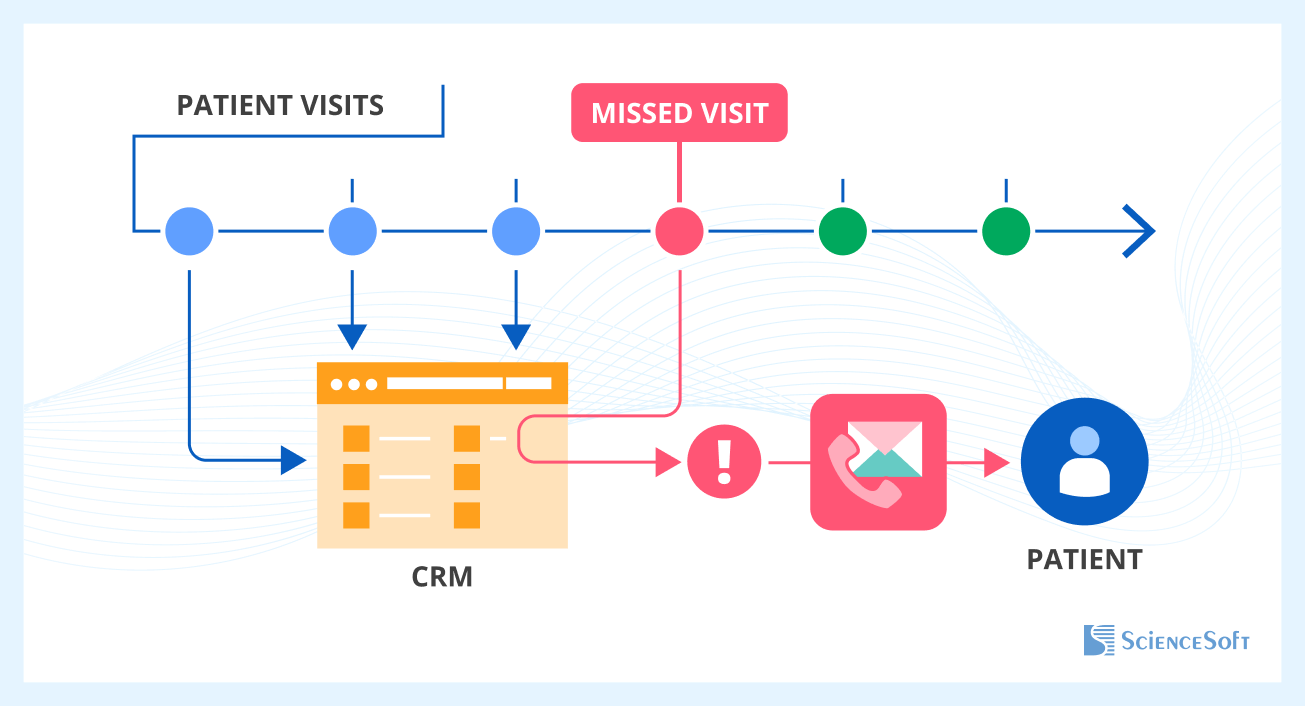
A well-tuned CRM for healthcare is the system to notify doctors about uncompleted stages of a care cycle and to suggest how to resume interrupted care in line with the predefined rules activated in the system. Complete profiles and communication histories of ‘undisciplined’ patients would help to decide on the best possible option to contact (via a direct email, a call from the care provider, etc.) and win them back, reducing the odds of a readmission or complication and driving higher revenues at the same time.
Try this demo to see how it works.
CRM and patient engagement
An informed patient is a step closer to recovery. At every stage of care delivery, a healthcare CRM would supply patients with personalized content via all the integrated channels, such as emails, a website, and a patient portal. It is especially important during the post-surgery convalescence at home when a patient may misinterpret symptoms or get anxious about his or her healing progress.
In practice, CRM takes a doctor’s place to a certain extent, by timely and professional communication of relevant information, whether through personalized website downloadables or handy brochures in a patient’s inbox (based on the information skimmed from the electronic medical records, as described above). This helps to sustain patients’ satisfaction with the quality of care and keep up warm, personal relationships with each and every one of them, whether it’s a dozen or a few thousand people.
CRM and patient satisfaction
In healthcare, no relationship can end with discharge. Regardless of the type of a patient’s condition, following up long after the last appointment helps both to sustain the quality of life and nurture patients’ loyalty (a true win-win for healthcare providers!).
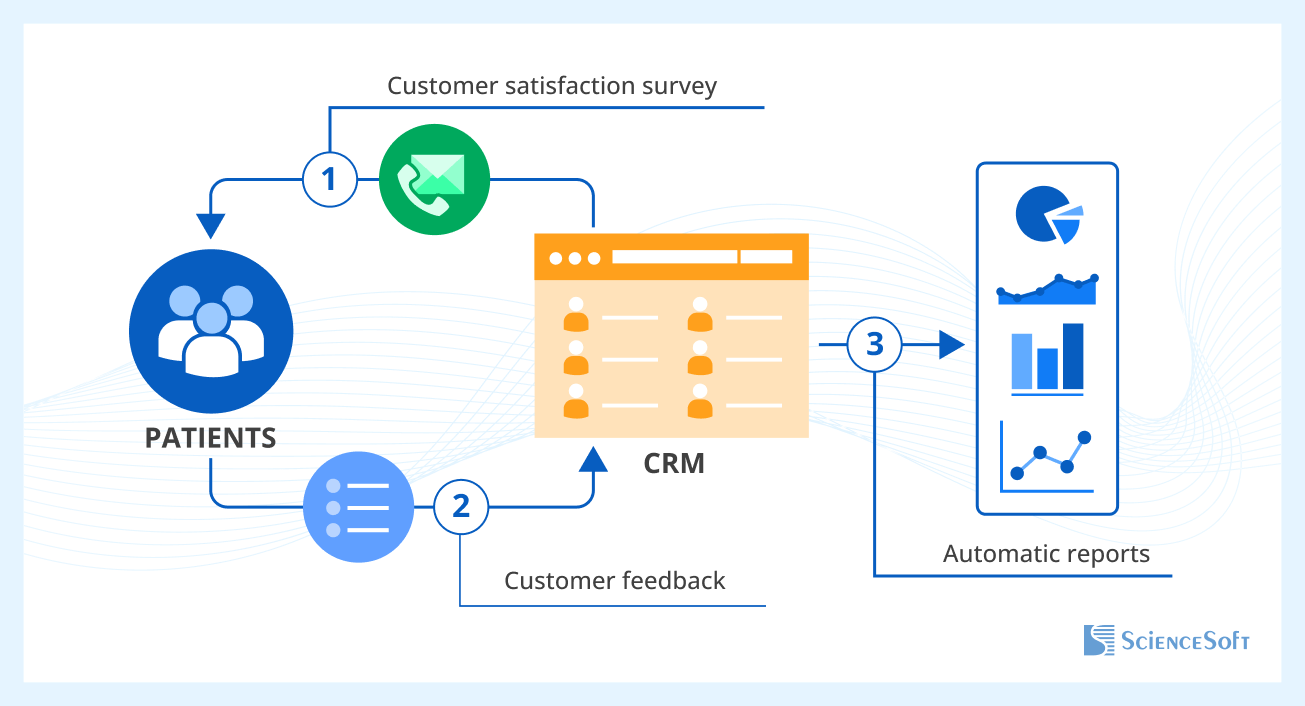
A healthcare CRM provides advanced capabilities for tracking a patient’s satisfaction, mood, and likelihood of referring their care provider to others. This information can be obtained either by an individual inquiry via a patient’s preferred communication channel or an automated survey sent out to specified patients. Most importantly, this information can be used to generate automatic reports on patient satisfaction, visible to executives and major decision-makers.
How to ensure secure data exchange with CRM
When US healthcare providers approach us with plans to connect their CRM and EHR systems, we treat HIPAA compliance as a core requirement that needs to be reflected in the integration design from the very start.
One of the first steps we usually take is narrowing down the scope of patient data that the CRM actually needs. In our projects, we typically limit this to appointment records, demographic data, patient consent flags, and perhaps summaries of recent diagnoses — enough to support outreach, personalization, and care coordination, but not so much that it introduces unnecessary risks. This way, CRM stays helpful without becoming a secondary storage of all patient data.
To maintain transparency around user activity, we help our clients set up audit logs on both EHR and CRM and standardize them for consistency. All user actions are logged with timestamps and user IDs. It’s better to consolidate these logs into a shared repository and apply cross-system correlation so administrators can trace full user sessions across the CRM and EHR. This kind of end-to-end audit trail proves especially useful during compliance checks and internal investigations.
For access management, we often recommend connecting both the CRM and EMR to a unified identity provider. That could mean integrating with an organization’s SSO setup using protocols like SAML. With this approach, a user’s permissions are defined centrally and enforced consistently, which helps prevent permission mismatches (like when a nurse loses access to one system but retains it in another). It also makes staff onboarding and offboarding much more secure and less error-prone.
Another point we focus on is securing the data in transit. Whether the integration involves direct API calls or a message queue, we make sure data is encrypted using TLS 1.2 or above, and that all endpoints enforce mutual authentication.
Consent management tends to be trickier, especially if the CRM and EHR handle it separately. To avoid conflicts, we usually go for a shared consent repository or a sync mechanism between the two systems. For instance, if a patient opts out of receiving reminders via the CRM, that preference gets automatically updated in the EHR too. This not only ensures compliance but also avoids awkward situations where a patient receives communications they explicitly declined.
Conclusion
Underestimated at the moment due to the industry’s bias towards electronic systems imposed by the government, a CRM for healthcare, however, opens up whole new opportunities when integrated with an EHR. Recognizing the latter’s crucial role in keeping and processing patients’ data, we tried to outline at least four areas where care providers can benefit from positive spillovers of the systems’ integration:
- winning patients at the pre-care stages
- resuming interrupted care
- stimulating patient engagement
- tracking their satisfaction with the quality of care
Compared to EHR, healthcare CRM shifts the focus from treatment to relationship management with effective and empathic communication at its core, regardless of how many patients you have. Giving in to a technology takes overcoming certain barriers, it’s true. But since healthcare IT is here to stay, it’s only a matter of months till competition will raise the bar and make automation of processes a recipe for survival (no pun intended).