Device-Connected Diabetes Monitoring Software
Capabilities, Development Tips, and Costs
Relying on 20 years in medical device software engineering and an ISO 13485 certification, ScienceSoft designs HIPAA-aligned architectures and data pipelines that allow for centralized and reliable device-based monitoring.
Diabetes Monitoring Software in a Nutshell
Diabetes monitoring software enables healthcare providers to continuously track glucose levels and other parameters of diabetes patients through connected CGMs, insulin pumps, and related devices. The software automatically collects, consolidates, and visualizes patient data, helping care teams identify trends, detect anomalies, and intervene early. By automating data collection and analysis, such solutions support more proactive, personalized diabetes management, improve adherence, and reduce the risk of complications between visits.
Custom diabetes monitoring software is a pragmatic choice for providers who need to manage multiple device brands and distinct care models within a single workflow. A tailored monitoring platform can encode device-specific processes (e.g., separate accuracy verification steps for each CGM type or different notification thresholds for inpatients versus outpatients), ensuring that all connected devices are monitored under the organization’s exact clinical protocols.
A custom solution can also address a broader range of quality reporting needs. With the growing emphasis on outcome-based reimbursement, platforms may need to aggregate and analyze CGM-derived metrics across patient cohorts (e.g., percentage of patients whose most recent glucose management indicator (GMI) is <8% or >9%) for submission to quality measurement systems or payers. Building these calculations directly into the data pipeline helps align monitoring results with reporting frameworks like HEDIS or internal performance dashboards.
In addition, a custom remote patient monitoring (RPM) platform can deliver stronger and more sustained patient engagement. It allows the provider to design personalized reminders, educational content, and escalation logic that reflect the clinic’s communication style, staffing patterns, and patient demographics. Tailoring these interaction flows helps reduce attrition and encourage continuous participation in long-term diabetes management programs.
- Implementation time: 4–12+ months.
- Development costs: $200,000–$600,000. Use our free calculator to get a tailored estimation for your initiative.
In-Demand Capabilities of Diabetes Monitoring Software
Below is a set of capabilities recommended by ScienceSoft’s consultants based on practical project experience.
Device data ingestion
Diabetes monitoring platforms can retrieve glucose readings and related parameters from vendors’ cloud repositories. The solution normalizes the data, validates its accuracy and provenance, and maps it to standard FHIR profiles to populate patient records in the EHR. Ingestion can occur in real time or in scheduled batches, depending on data availability and clinical needs.
Monitoring and alerts
A custom solution can periodically check glucose readings and derived indicators against configurable thresholds. Rules may include simple limits, rate-of-change conditions, or aggregated patterns over a set period. When triggered, alerts can be routed to the appropriate clinician or care coordinator’s EHR interface, with configurable escalation logic and suppression settings.
Device management
An integrated module can display device connectivity and performance indicators (e.g., battery level, signal stability, and synchronization frequency) for patients under monitoring. Care teams can monitor these metrics via the EHR or asset monitoring systems and, if needed, submit service requests to the device manufacturer or technical support. This visibility helps maintain data continuity and ensures the timely resolution of technical issues.
Clinician-facing analytics
Clinical dashboards display glucose trends, cohort filters, and standardized summaries built from device data. These summaries can include metrics such as Time-in-Range, Time-Below-Range, and Glucose Management Indicator, as well as basic data quality indicators. The analytics layer can also support deterministic clinical calculators based on established glucose-insulin models, helping clinicians evaluate therapy effectiveness and document decisions.
Patient engagement
Patients can log contextual information such as meals, activity, or medication adherence via EHR-integrated portals or companion apps. With added telemedicine functionality, these interfaces can also facilitate communication between patients and care teams, allowing clinicians to provide feedback, educational resources, or care instructions. Built-in reminders and gentle nudges can prompt patients to record readings, follow care plans, or attend scheduled check-ins.
Patient-facing analytics
Within the portal or app, patients can view their own data in dashboards and widgets that display glucose trends, averages, and daily or weekly summaries. Visualizations help them understand how lifestyle choices affect glucose stability and reinforce adherence to treatment plans. These interfaces are read-only, focusing on insight and motivation rather than therapeutic guidance, and can mirror clinician metrics such as Time-in-Range for consistency of interpretation.
Population health reporting
Custom solutions can analyze device-generated data and calculate quality reporting metrics across patient cohorts. For example, they can determine the percentage of monitored patients whose most recent results meet or exceed CMS- and NCQA-defined thresholds (e.g., GMI <8% or >9%). The output will show the numerator, denominator, and exclusions along with the final result for full traceability. Structured files can be de-identified and exported using QRDA or registry-specific formats when required.
Security and compliance
Custom diabetes monitoring implementations can comply with all necessary jurisdictional and sectoral security controls from the design stage. Access is role-based and recorded through immutable, time-stamped audit trails that meet HIPAA and 21 CFR Part 11 expectations. All data is encrypted in transit and at rest, while configurable de-identification pipelines support secure analytics and secondary data use.
How AI Capabilities Can Enhance Diabetes Monitoring
Smart historical analysis
Generative agents can help clinicians quickly interpret historical data and perform ad hoc analytics using natural language prompts. For example, when asked to “find patients with suboptimal Time-in-Range over the past three months" or "visualize the correlation between weight, physical activity, and glucose levels over the past six months," the agent identifies relevant datasets, performs the analysis, and presents the output as a human-readable summary or an interactive chart without requiring predefined queries or manual data manipulation.
Clinical documentation
LLM-based agents integrated into the EHR can draft structured documentation of diabetes monitoring encounters. They can transcribe clinician dictation via speech-to-text, access device data, and extract other relevant information from EHR fields to compose RPM progress notes, monthly summaries, and patient letters. Using RAG over approved templates and policies, the assistant assembles content in standardized formats like SOAP notes. All outputs should remain editable and require clinician review and approval, preserving documentation quality and regulatory compliance.
“Talk with the manual” for patients
Patients using connected devices may encounter common technical issues such as connection drops. A chatbot integrated into the EHR-connected patient app can use RAG to extract relevant troubleshooting steps from vendor-provided documentation specific to the devices used by the clinic. It then delivers clear, step-by-step instructions in plain language. If the issue persists, the chatbot can guide the patient in preparing a detailed service request for tech support.
Quality reporting
LLM-driven agents can assist with the narrative portion of quality reporting. Based on structured metric outputs (e.g., Time-in-Range trends across monitored patients), they can generate readable summaries that describe key outcomes for specific cohorts. The agent’s capabilities can be extended to draft entire structured reports. By retrieving template instructions via RAG, it can pre-fill key sections in the correct order. All outputs remain subject to human verification and institutional approval within the EHR.
Diabetes Monitoring Software Development Tips
1
Start with 1–2 vendor integrations for faster rollout
ScienceSoft recommends beginning with a minimal viable product that connects a few major device vendors via their public APIs or through a trusted aggregator. The software can pull and normalize validated readings, link them to patient records in the EHR, and display glucose trends and alerts within the clinician workflow. Early releases should focus on data reliability, identity reconciliation, and clinician usability before expanding to more devices, richer analytics, and multi-cohort dashboards. This approach helps organizations prove value quickly while avoiding unnecessary infrastructure complexity.
2
Stay below the FDA threshold with human-in-the-loop analytics
All analytical and decision-support components should function in an advisory capacity. ScienceSoft recommends designing outputs that include confidence scores, reasoning chains, and references to data sources, so clinicians can independently review and confirm recommendations. This human-in-the-loop pattern qualifies as Non-Device CDS under FDA guidance, avoiding the need for premarket clearance while maintaining clinical transparency. The same approach can apply to any AI-generated summaries, ensuring that clinicians remain the final authority for all therapeutic decisions.
3
Apply low-code where it delivers quick wins
Low-code tools such as Microsoft Power Apps can accelerate the development of administrative dashboards, consent logs, and population-level review interfaces that change frequently. These modules can easily connect to your EHR or analytics back end via secure APIs and work well for iterative workflows like quality-report preparation or outreach management. Patient- and clinician-facing experiences, however, are best kept fully custom to ensure high performance, accessibility, and brand consistency within the EHR ecosystem.
4
Keep API data ingestion reliable
When connecting device vendor platforms or data aggregators, the monitoring module needs to collect readings efficiently and without interruptions. Most vendor APIs limit how much data you can pull at once (e.g., only 30 days of glucose data per request), so the system should fetch information in smaller batches until it’s fully updated. To keep connections stable, it’s useful to include retry logic if a request fails and an automatic slowdown if an API warns of too many requests. Some vendors support webhooks or push notifications when new data is available. Using these signals instead of constant polling saves computing time and reduces costs.
5
Don’t overstretch your EHR with incoming data
Decide early which data elements should become discrete EHR entries (for example, glucose observations or flowsheet rows) and which are better delivered as embedded widgets or reports. Writing too many granular data points can strain EHR throughput and clutter clinician views. ScienceSoft advises aligning FHIR profiles with your EHR vendor’s guidelines and establishing a consistent mapping strategy for device metadata and derived metrics. For population reporting, schedule periodic Bulk FHIR or data warehouse updates rather than attempting continuous writes.
Technologies We Use to Build Secure and Efficient Patient Monitoring Software
ScienceSoft: An Experienced Partner for Diabetes Monitoring Software Development
- Since 2005 in healthcare IT and remote patient monitoring software development.
- Since 2012 in IoT and cloud technologies.
- Mature quality management and security management systems backed by ISO 13485, ISO 9001, and ISO 27001 certifications.
- Proficiency in achieving compliance with the requirements of HIPAA, GDPR, 21st Century Cures Act, 21 CFR Part 880, and more.
- Hands-on experience with healthcare interoperability standards (HL7, FHIR, CCDA, XDS/XDS-I) and clinical coding vocabularies (e.g., ICD-10, CPT, SNOMED CT, LOINC, RxNorm).
- 20+ principal architects balancing compliance and efficiency in medical software architectures.
Our awards, recognitions, and certifications
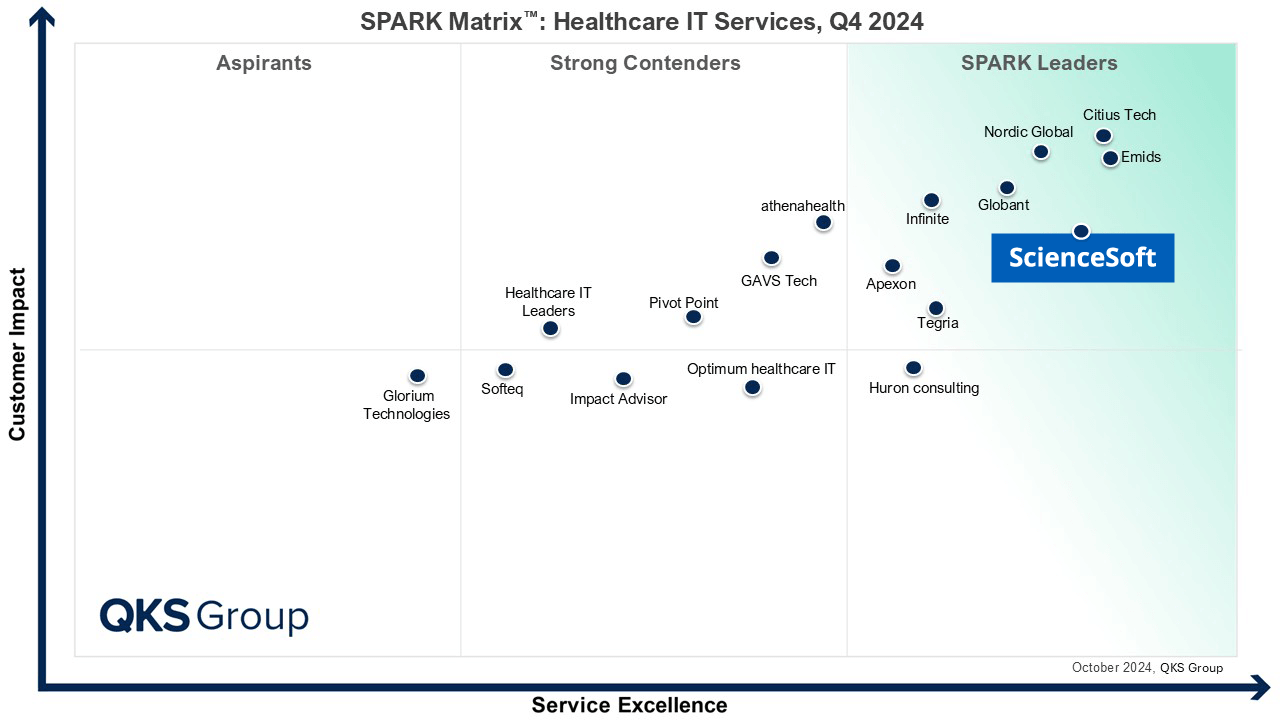
Featured among Healthcare IT Services Leaders in the 2022 and 2024 SPARK Matrix
Recognized for Healthcare Technology Leadership by Frost & Sullivan in 2023 and 2025
Named among America’s Fastest-Growing Companies by Financial Times, 4 years in a row
Top Healthcare IT Developer and Advisor by Black Book™ survey 2023
Four-time finalist across HTN Awards programs

Named to The Healthcare Technology Report’s Top 25 Healthcare Software Companies of 2025

HIMSS Gold member advancing digital healthcare
ISO 13485-certified quality management system
ISO 27001-certified security management system
Development Costs of Device-Connected Software for Diabetes Monitoring
From ScienceSoft’s experience, developing device-connected diabetes monitoring software may cost around $200,000–$600,000+.
Estimate the Cost of Your Remote Patient Monitoring Solution
Please answer a few questions to help our healthcare IT consultants accurately assess your needs and provide a cost estimate quicker.
Thank you for your request!
We will analyze your case and get back to you within a business day to share a ballpark estimate.
In the meantime, would you like to learn more about ScienceSoft?
- Project success no matter what: learn how we make good on our mission.
- Since 2005 in healthcare IT services: check what we do.
- 4,200+ successful projects: explore our portfolio.
- 1,400+ incredible clients: read what they say.







