Care Management Software
Features, Architecture, Costs
In healthcare IT since 2005, ScienceSoft builds robust, regulatory-compliant software to let managed care organizations (MCOs) efficiently supervise the delivery of high-quality care and control care costs.
Care management software is used by managed care organizations (MCOs) to oversee and coordinate patient care delivery across the provider network, track service utilization, ensure diagnosis correctness and relevance, and more.
Note: This page describes care management software intended for managed care organizations (MCOs) such as health maintenance organizations (HMOs), exclusive provider organizations (EPOs), preferred provider organizations (PPOs), and point-of-service plans (POS). If you are interested in a solution for synchronizing the efforts of care teams, healthcare institutions, and other entities involved in patient care, feel free to explore our dedicated guide on care coordination software.
According to IMARK Group, the care management software market is expected to reach $46 billion by 2033. The major market drivers include the increased percentage of chronic diseases, the rising shift toward value-based care, the increasing adoption of ML/AI techs, and the promotion of digital health tools by government organizations.
Custom care management software development is an optimal choice when diverse data exchange formats and protocols used by the involved providers need to be standardized. Custom solutions also provide more flexibility in the choice of ML/AI-powered features, such as analytics for identifying care gaps and assessing provider performance.
- Implementation time: 6 to 18+ months.
- Common integrations: EHR/EMR, LIS, RIS, HIE, a clinical decision support system (CDSS), telehealth platforms, a patient portal.
- Costs: $600,000–$5,000,000+, depending on the solution's complexity. Answer a few questions about your business needs to get a custom quote from our consultants.
Popular Features of Care Management Software (CMS)
Provider network management
CMS should maintain a database of all the in-network and partner providers and a catalog of their services. It should also support provider contract management, credentialing (tracking licenses and certifications), and onboarding. The system must support the relevant data exchange standards (e.g., HL7 v2/v3, FHIR with USCDI-aligned payloads) to enable interoperability with provider systems and secure data exchange.
Utilization management
Utilizing provider claim data (e.g., services rendered, costs), the system can help track service utilization across providers (e.g., types of delivered services, frequency of visits to a particular facility) and generate case review alerts (e.g., on possible exceeding of service utilization). CMS can also have automation capabilities for handling pre-authorization requests from providers.
Checking treatment correctness
Analyzing data on the provided services, the system can assess diagnosis correctness and procedure relevance by checking whether diagnostic codes (e.g., from ICD-10) align with corresponding procedure codes (e.g., from CPT). Optionally, SNOMED CT may be used where condition lists need normalization.
These can be tools for collaborative care plan development and editing, referral management, discharge planning, readmission risk assessment, preventive care management, and more.
Care management analytics
CMS can include analytics tools to monitor provider performance (e.g., health outcomes, utilization rates) and identify inefficiencies such as care gaps or overutilization of services. CMS can also help assess provider profiles (e.g., availability, capacity) and pinpoint high- or underperforming providers. Such software can also feature predictive analytics capabilities (e.g., to forecast care costs) and create automated reports for submission to regulatory bodies (e.g., to CMS in the US) in compliant formats.
CMS can have dedicated patient portals and apps to facilitate communication with patients. These tools can be used to notify patients of claim status, send reminders about appointments and follow-up activities, and more. Patient engagement can also offer educational healthy lifestyle content (e.g., self-check guides, videos, articles) and provide personalized recommendations on preventive care services (screenings, check-ups, vaccinations, etc.) or lifestyle changes.
Sample Architecture of Care Management Software
Below, our solution architects provide a sample architecture of a care management solution that lets managed care organizations oversee care delivery and control service utilization and costs across the provider network. You can also explore a sample architecture of a custom care coordination solution intended for synchronizing the efforts of care teams within healthcare institutions.
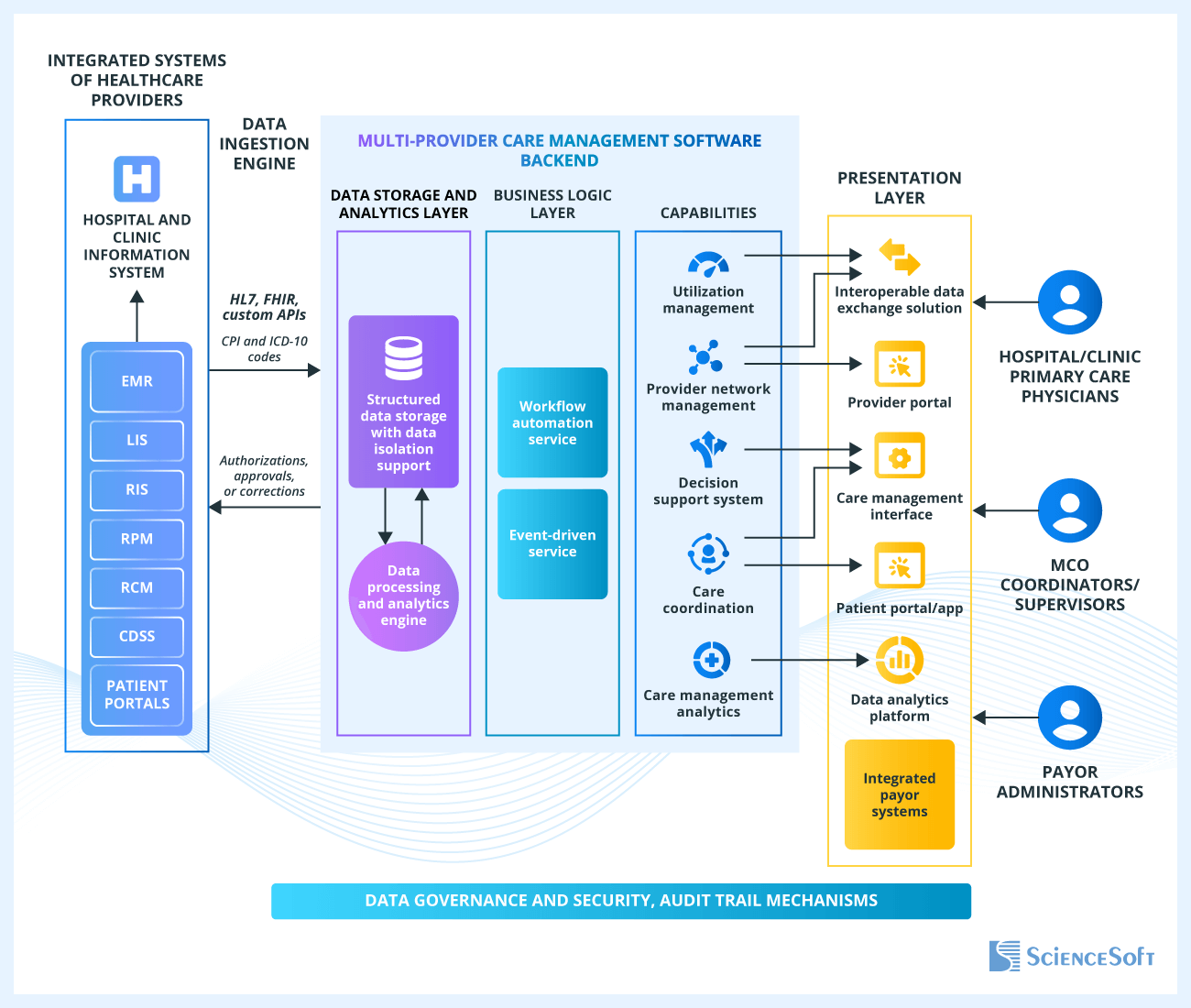
The software gets data from the hospital information systems (HIS) of providers. HIS incorporates data from various back-office software, including EHR/EMR, revenue cycle management software (RCM), laboratory information systems (LIS), and more. The means of integrating CMS with HIS may include data exchange protocols and standards, such as HL7 v2/v3 and FHIR (USCDI-aligned where applicable), CCDA for document exchange, or custom APIs. Claims data can be ingested via HIPAA X12 837/835.
The software backend is built using a multi-provider model where each provider’s data is managed independently. This can be achieved through dedicated database schemas within the data storage, dedicated or serverless data processing pools, customizable operational database templates, tools for tracking provider-specific usage metrics (e.g., API calls), and more.
Data from HIS is automatically ingested and preprocessed via a data ingestion engine on a scheduled and event-driven basis and is fed into the long-term data storage or sent to analytics layer and data processing engine for further processing and analysis.
The business logic layer features the workflow automation service that automates workflows across provider systems e.g., updating a patient medical history after a corresponding record was updated in the provider’s EHR. The event-driven service acts locally, in the providers’ systems. In the scenario above, a notification would be sent to the employees involved in managing care of a particular patient.
Users interact with the software via dedicated apps and portals. For example, primary care physicians (PCPs) at clinics communicate with MCO coordinators via provider portals; MCO coordinators can track service utilization via a care management interface and exchange data with providers via an interoperable data exchange solution. Communication with patients is enabled via patient portals and apps.
By integrating their systems with care management software, payors can access data on service utilization and reimbursement and take preventive or corrective measures to optimize care costs.
Security mechanisms for care management software typically include data encryption at rest and in transit, identity and access management, role-based user access control (RBAC), audit trails and logs, and more.
How to Develop Care Management Software
Care management software development is needed to let MCOs benefit from the smooth integration of software systems across multiple healthcare providers. Below, our healthcare consultants provide a general overview of key steps for developing a custom care management system. In the actual project, some of the steps may differ depending on your organization’s needs.
1.
Business analysis and requirement engineering
At this stage, business analysts communicate with the stakeholders (e.g., MCO coordinators, payor administrators) to elicit the details required for shaping functional and non-functional software requirements. The specialists find out the types and number of healthcare organizations the CMS solution will cover, care management use cases it will support, regulations it should comply with, and the solutions it will integrate with (e.g., providers’ EHRs by Epic or Cerner).
2.
Integrations and architecture design
At this step, solution architects decide on the integration strategy. They define the relevant data exchange standards and protocols (e.g., HL7 v2/v3, FHIR with USCDI-aligned resources, CCDA for document exchange, HIPAA X12 837/835 for claims). The specialists also analyze providers’ software (e.g., EHRs, LISs) that the CMS should integrate with and see if there are ready-made APIs (e.g., either offered by software vendors or cloud service providers) or if custom API development is needed. Where clinical data normalization is required, terminologies such as ICD-10, CPT, LOINC, RxNorm, and SNOMED CT are considered.
The experts analyze system requirements for scalability, elasticity, performance, availability, and other parameters, and choose technologies that can satisfy these requirements at an optimal cost-to-benefit ratio.
3.
UX/UI design
UX and UI designers create workflows and visual elements that enhance the solution’s usability and streamline the completion of tasks for the defined user roles. For instance, MCO coordinators may benefit from dashboards that give a 360-degree view of service and resource utilization with the capability to drill down into details. If an accompanying mobile app for on-the-go care management is planned, UI designers create simplified interfaces for smaller screens.
4.
Development and testing
Development and testing teams often work in parallel to better coordinate efforts and fix defects as soon as they are detected. The specialists can also go for QA automation when feasible. Infrastructure engineers implement DevOps practices.
In ScienceSoft’s experience, combining ready-made components from reputable cloud providers (e.g., AWS, Microsoft, Google Cloud) with custom elements can speed up development by 2-20 times and cut development costs by up to 50%. For example, Microsoft Cloud has pre-built elements designed specifically for care management. They include templates for care plans and patient profiles that can be either fully reused or enhanced with custom elements to accommodate unique patient conditions, care plan activities, or organizational requirements. Furthermore, Microsoft offers a ready-made patient portal that can be directly incorporated in the solution instead of developing one from scratch.
5.
Deployment and support
The development team deploys the care management software and monitors its performance. Developers also deliver exhaustive software documentation, including maintenance guides, instructions on API usage, and user training materials.
How Much Does It Cost to Develop Care Management Software?
The costs of care management software development may range from $600,000 to 5,000,000*. The major cost factors include the complexity and range of its features, the number of targeted institutions and supported users, and integration capabilities.
*The range is for CMS designed for managed care organizations (MCOs). If you're planning to build a system for synchronizing care within medical institutions, check care coordination software costs.
|
|
Core solution |
Advanced solution |
|---|---|---|
|
Features
|
|
|
|
The number of organizations that will be using the software
|
Up to 100 |
Up to 500 |
|
The number of supported users
?
E.g., PCPs, MCO coordinators, payor administrators. |
Up to 10,000 |
Up to 100,000 |
|
A patient portal
|
Up to 1,000,000 patients |
More than 1,000,000 patients |
|
Analytics and reporting complexity
|
|
|
|
Software costs
|
$600,000–$1,500,000 |
$1,500,000–$5,000,000 |
Why Develop Your Care Management Software With ScienceSoft
- Since 2005 in healthcare IT and custom healthcare software development with 150+ successful projects in the industry.
- Experience in achieving compliance with HIPAA, GDPR, 21st Century Cures Act, PDPL, PIPEDA, and other regulations.
- Since 1989 in AI and machine learning to build reliable predictive analytics and automation features.
- Proficiency in HL7 v2/v3, FHIR (USCDI-aligned), CCDA, HIPAA X12 837/835, DICOM, ASTM, and other healthcare data exchange protocols and standards.
- ISO 9001-certified quality management system and ISO 27001-certified information security management system.
- Among the leaders of the healthcare IT services market in the 2024 SPARK Matrix, according to Quadrant Knowledge Solutions.
Our awards, recognitions, and certifications
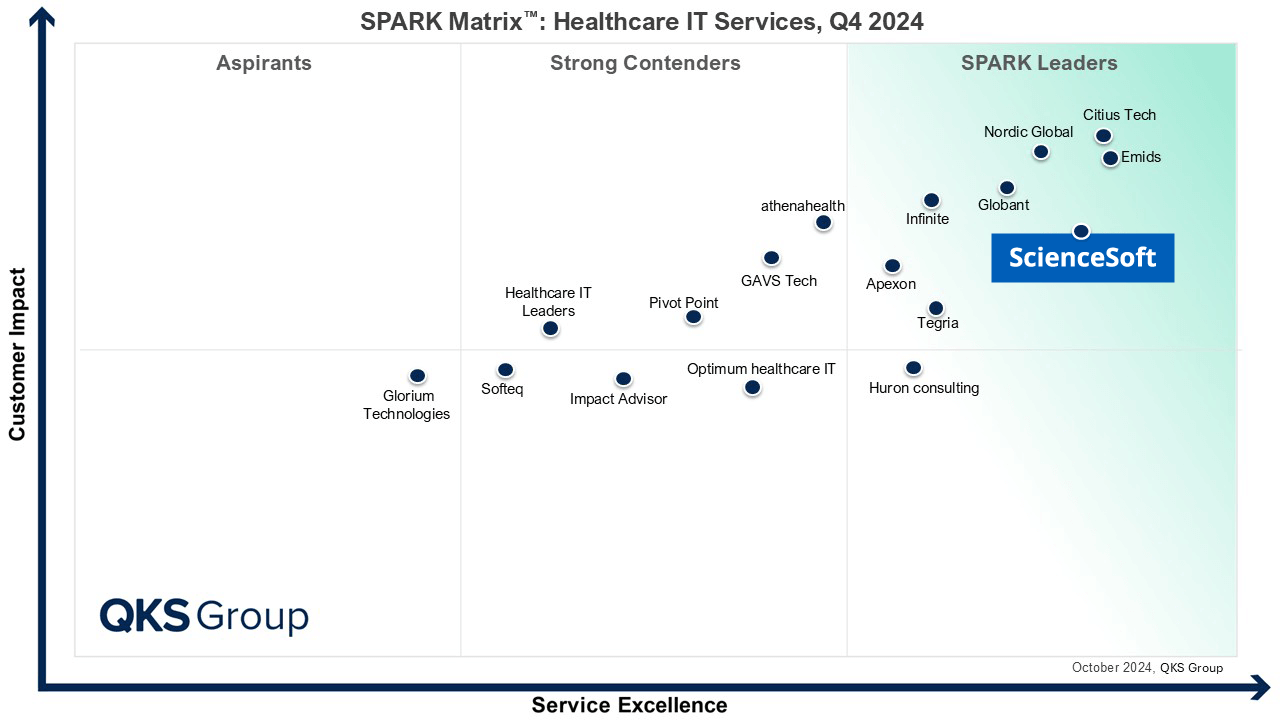
Featured among Healthcare IT Services Leaders in the 2022 and 2024 SPARK Matrix
Recognized for Healthcare Technology Leadership by Frost & Sullivan in 2023 and 2025
Named among America’s Fastest-Growing Companies by Financial Times, 4 years in a row
Top Healthcare IT Developer and Advisor by Black Book™ survey 2023
Four-time finalist across HTN Awards programs

Named to The Healthcare Technology Report’s Top 25 Healthcare Software Companies of 2025

HIMSS Gold member advancing digital healthcare
ISO 13485-certified quality management system
ISO 27001-certified security management system



