Wearable Biosensors for Effective Remote Patient Monitoring
Editor’s note: Alena discusses the diverse applications and success factors of wearable biometric sensors for remote health monitoring. If you are looking for a reliable vendor to bring an effective solution for your wearable biosensors, check ScienceSoft’s offering in medical device software development.
Recent studies show that the wearable biosensors market is growing and will reach $9.26 billion by 2030. And my experience with wearable devices and patient monitoring projects (for example, a mobile heart rate tracking app) shows that only those producers of wearable biosensors who augment their sensors with cloud applications will remain competitive in the growing market. Still, many manufacturers experience software-related technology gaps, so they are wary of adding a cloud application to their products, fearing to harm future users.
In the article, I explain why enriching your wearable biosensors with a cloud biosensor app is a good idea, refute widespread concerns you may have about it, and show how collaboration with a software vendor can be of help in the task.

How Wearable Biosensors Are Used Today
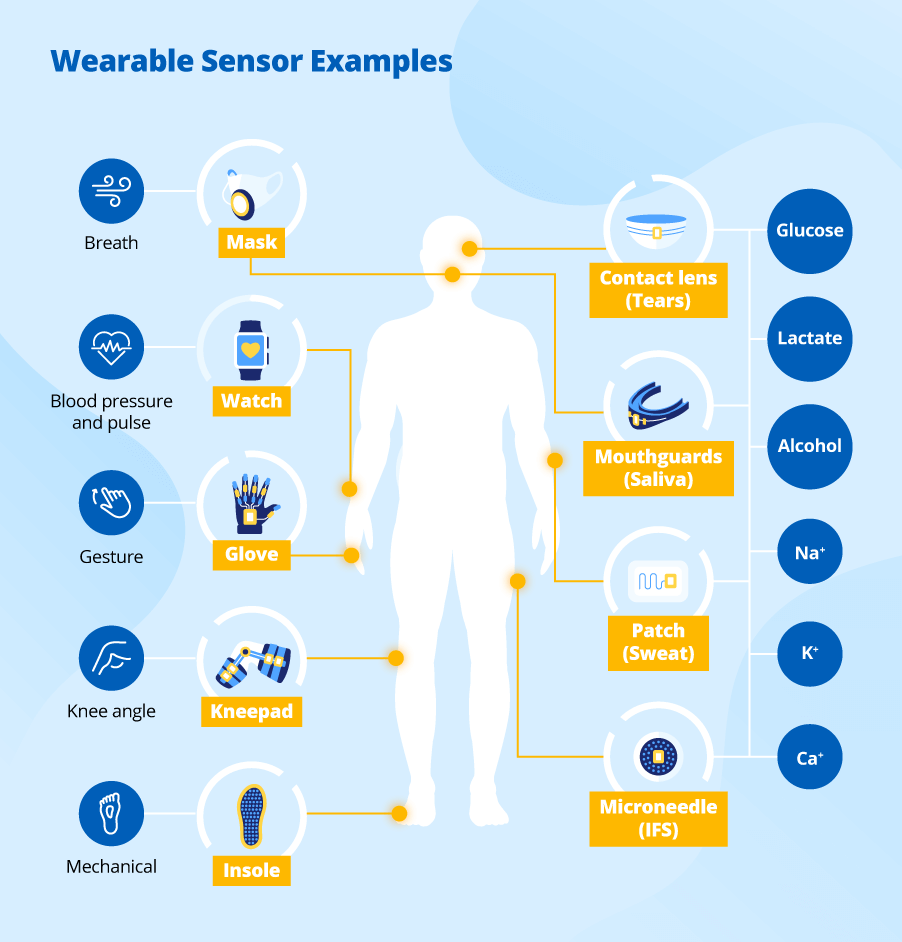
Modern biosensors support a wide range of health monitoring scenarios. In chronic disease management, continuous glucose monitors help diabetic patients avoid finger-prick tests and view real-time glucose levels on their mobile phones. In post-operative care and physical therapy, motion-detecting biosensors enable remote monitoring of joint angles and gait, providing therapists with accurate recovery data without the need for frequent in-person visits. In sport and fitness training, wearable biosensors can track respiration rates, lactate thresholds, and electrolyte levels to optimize training and reduce the risk of overexertion.
How Can Your Solution Look?
Below, you can see the simplified architecture of a typical cloud app solution for wearable biosensors that ScienceSoft offers to its customers. The standard IoT solution architecture is described in more detail in the article by my colleague Alex Grizhnevich.
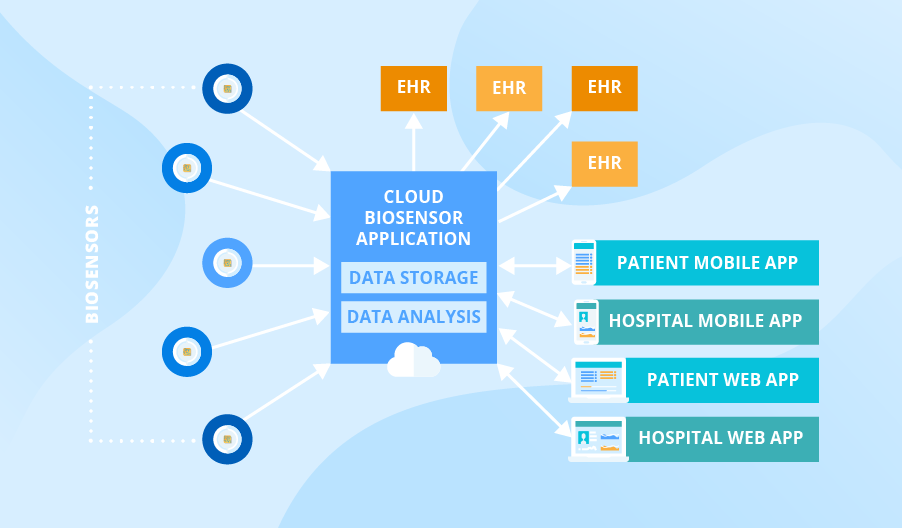
Data gathered by biosensors goes directly to the HIPAA-compliant cloud biosensor application, where it is stored and analyzed. This cloud application feeds analyzed patient data to the EHR systems of care providers, where it can be accessed and managed. All data from the app may be available via patient/hospital mobile and web applications, which facilitates access to clinical information for patients and medical staff.
How Comfort and Usability Affect Biosensor Adoption
Even the most capable biosensor won't succeed if users don’t want to wear it. Comfort, aesthetics, and ease of use are as important for widespread adoption as clinical effectiveness. Older adults often require larger fonts, physical buttons, clear user instructions, and intuitive navigation to feel confident using digital health devices. Meanwhile, fitness-focused users expect lightweight materials, water resistance, and seamless syncing with their mobile fitness apps.
From the software side, we focus on making sure the device fits naturally into the user’s daily routine. In some cases, this means optimizing sampling frequency and transmission logic to conserve battery and extend usage without recharging. In other cases, it’s about ensuring the interface can scale across different device types. For example, smartwatches often require dedicated app development or significant adaptation of existing mobile apps.
How Can Your Concerns About Wearable Biosensor Software Be Fought Off?
You are likely to have certain concerns regarding the development of cloud software for your wearable biosensors. For example, the most widespread worries of ScienceSoft’s customers are about harming the patients, violating personal data security, and having poor awareness about end-customer needs. Let’s see how they can be mitigated in collaboration with a dedicated vendor.

Harming patients is hardly probable
My customers often worry that incorrect data collection or errors in algorithms can lead to inaccurate actions of a wearable device and wrongly suggested treatment for patients. For example, the app connected to the wearable glucometer detects an abnormal blood sugar level and notifies a patient to inject insulin, but in fact, the blood sugar level is within normal limits.
First of all, I’d like to point out that wearable device software is not supposed to replace doctors. Its main goals are:
- Monitor patients’ activity and health conditions remotely.
- Provide better patient data visibility via live reports.
- Timely alert a doctor about a possible problem to increase treatment quality and speed.
However, low-quality data and algorithm errors may indeed affect the quality of a doctor’s decisions. To minimize such a possibility, you may use recent advances in artificial intelligence, machine learning, and big data processing technologies to automate data recording/processing and support automatic monitoring with the help of a reliable vendor. These technologies also help achieve better accuracy of sensors.
Furthermore, I insist on providing quality assurance at different levels (biosensor, data ingestion, and algorithms). A thorough approach to QA that covers various types of testing (functional testing, performance testing, and compatibility testing) allows for minimizing the possibility of harming patients.
Security issues are manageable
The issue of data security in the healthcare industry is an acute one, since, for example, leakage of patient data can lead to huge financial and reputational losses. To improve data security, I suggest adhering to one of the main cybersecurity principles well formulated by Dmitry Kurskov, Head of Information Security Department at ScienceSoft:
“Applying cybersecurity measures once and forgetting about them forever is not a good strategy. The system security level should be regularly monitored, assessed, tested, and improved.”
Below, you can find a list of security measures relevant for wearable biosensor projects:
- Using security-first software architecture patterns.
- Using relevant permission settings.
- Performing regular vulnerability assessment and penetration testing.
- Conducting continuous network monitoring.
Poor awareness about customer needs is solvable
As my experience shows, it is difficult for producers of wearable biosensors to predict what functionality customers will need in software for wearable sensors besides the remote monitoring of patient health conditions and the data collection and processing.
As a business analyst and healthcare IT consultant, I believe that a thorough analysis of user needs and feature prioritization can help make the solution's feature set viable. Also, you should design your wearable biosensors software to cater to the evolving needs and goals of healthcare organizations and their patients. For that, I advise you to ensure that your future application is easily customizable so that buyers of wearable devices can adjust the system to their particular requirements.
What Growing Adoption Rates Tell Us About the Future of Biosensors
Wearable biosensors are no longer niche gadgets. With the current advancements in device and software usability, patients are now more open to using biosensors, not only in clinical environments but also in everyday life. One study involved 11 individuals with chronic stroke who used a wearable wristwatch device for home-based upper limb telerehabilitation. The System Usability Scale showed a high mean score of 84.3 out of 100, which indicates above-average and “excellent” usability, along with the 91% adherence rate. The participants also appreciated the possibility of operating the device with their phone, highlighting its convenience.
Wearable biosensors in healthcare are steadily gaining trust and acceptance. That’s the result of thoughtful design, both on the hardware and software side, and a clear signal that this technology is here to stay.
Enhance Health Journeys With Wearable Sensors
Indeed, building a medical device network for biosensors is not an easy undertaking. It requires skills in building a secure and scalable IoT architecture, big data storage and analytics, cloud development, and more. I believe that with those competencies in place and with a thought-out software development and QA strategy, all major risks like harming patients, violating personal data privacy and having poor awareness about end-customer needs can be mitigated. If you aren’t sure your competencies fit this list or if you want to know more details on how to avoid the major problems in your specific case, let me know.

