Revenue Cycle Management Software (RCM)
Architecture, Development Steps, Costs
In custom healthcare software development since 2005, ScienceSoft engineers secure, regulatory-compliant systems that automate revenue management processes, enhance billing and coding accuracy, and increase transparency of point-of-service payments.
Revenue cycle management software (RCM) is needed to streamline and automate patient registration, charge capture, coding, billing, claim submission and tracking, denial management, revenue recognition, and other RCM activities.
According to Grand View Research, the global RCM market was estimated at $306.8 billion and is projected to grow at a CAGR of 11.39% from 2024 to 2030. The adoption of revenue cycle management in the healthcare industry is driven by the growing need to optimize hospital workflows and achieve greater efficiency in ensuring patient satisfaction and optimizing operational expenses.
Custom healthcare revenue cycle management software is a popular choice among providers that aren’t satisfied with out-of-the-box RCM solutions. Typically, they need to accommodate complex revenue models, integrate RCM with diverse back-end systems, including legacy software, and meet specific compliance requirements. Custom solutions also provide an opportunity to implement tailored ML/AI-powered analytics — for example, to predict claim denials, forecast reimbursement timelines, and identify patient payment risks.
- Implementation time: 6 to 18+ months.
- Common integrations for RCM: EHR/EMR, practice management software, HIE portal, insurance providers portals, claims clearinghouse, banking systems, payment gateways, Medicare/Medicaid APIs, ICD/CPT updates providers, patient portals and apps.
- Costs: $500,000 to $2,500,000+, depending on the solution's complexity. Use our free online calculator to get a custom quote from our consultants.
RCM Features in High Demand
Patient registration and eligibility checks
Using data from EHR/EMR, payors’ systems, and online pre-registration forms, RCM software collects and verifies the information needed to support financial processes, including patient demographics and insurance policy details. It can automatically verify the patient’s insurance coverage and perform eligibility checks for specific services. Some RCM solutions also integrate with intake systems to confirm patients' billing consents and payment authorizations.
Charge capture and coding
RCM software should feature electronic charge tickets or forms that can automatically capture clinical data from EHR/EMR and allow for manual data entry. RCM should also have built-in coding guidelines (e.g., ICD-10, CPT codes) to facilitate code selection for diagnoses and procedures. Advanced systems with AI modules can provide code suggestions and flag potential coding errors.
Claim management
Well-integrated healthcare RCM solutions can automatically submit claims, track payments against submitted claims, send updates on claim adjudication status, and post remittances to patient accounts. Built-in claim scrubbing tools help to flag incorrect or missing information before submission, reducing denial rates. Some RCMs can also track and categorize denied claims and appeals, including the reasons for denial.
Prior authorization
RCM software can feature workflows for streamlining prior authorization, e.g., via task assignment to staff based on roles and availability, reminders for submission and follow-up dates, and ready-to-use request templates and checklists. Such solutions can also automate prior authorization by pre-populating forms with patient and service data and submitting electronic requests to payors.
Patient billing
RCM solutions streamline billing for all out-of-pocket payments, including co-pays, deductibles, co-insurance, and non-covered services. They can generate patient statements with clear breakdowns of amounts due and available payment options and help create payment plans. Advanced solutions enable complete billing cycle automation from invoice generation and delivery to reminders on outstanding balances.
RCM software helps prevent revenue leakage and accelerate cash flow by increasing coding accuracy and automating processes such as pre-authorization, claim management, and denial resolution. RCMs can also feature tools for revenue tracking and recognition (e.g., automated reconciliation of billed versus paid amounts).
Clearinghouse integration
Integration with a clearinghouse system allows for more automation capabilities throughout the revenue cycle, including claim submission, real-time eligibility checks, and claim tracking. The clearinghouse checks claim accuracy and completeness and facilitates claim management across multiple payors.
An intelligent revenue analytics module can forecast revenue and predict potential denials. It can help detect revenue cycle bottlenecks, identify reasons for claim denials or payment delays, find trends in patient payment behavior to improve collections, and more. BI modules can also generate reports for executives and regulatory bodies (e.g., on quality assurance and regulatory compliance). Advanced RCM solutions can feature BI chatbots that provide predictions and reports based on natural-language queries.
Fraud management
Machine learning and AI-powered mechanisms can detect suspicious patterns and events (e.g., duplicate billing, upcoding, non-typical billing rates, unusually high-cost procedures) and generate corresponding alerts. RCM in healthcare can also contain capabilities for automated compliance checks, including optional features powered by blockchain (e.g., immutable audit trails).
Tools for communication with payors
A user-friendly RCM solution should feature secure direct messaging mechanisms to enable protected communication with payors directly from the RCM interface. Allowing parties to discuss the claim management process, such tools promote faster settlements and improve collaboration between payors and healthcare providers.
Sample Architecture of Revenue Cycle Management Software
Below, our software architects provide a sample RCM architecture depicting application modules and core technology components that power them.
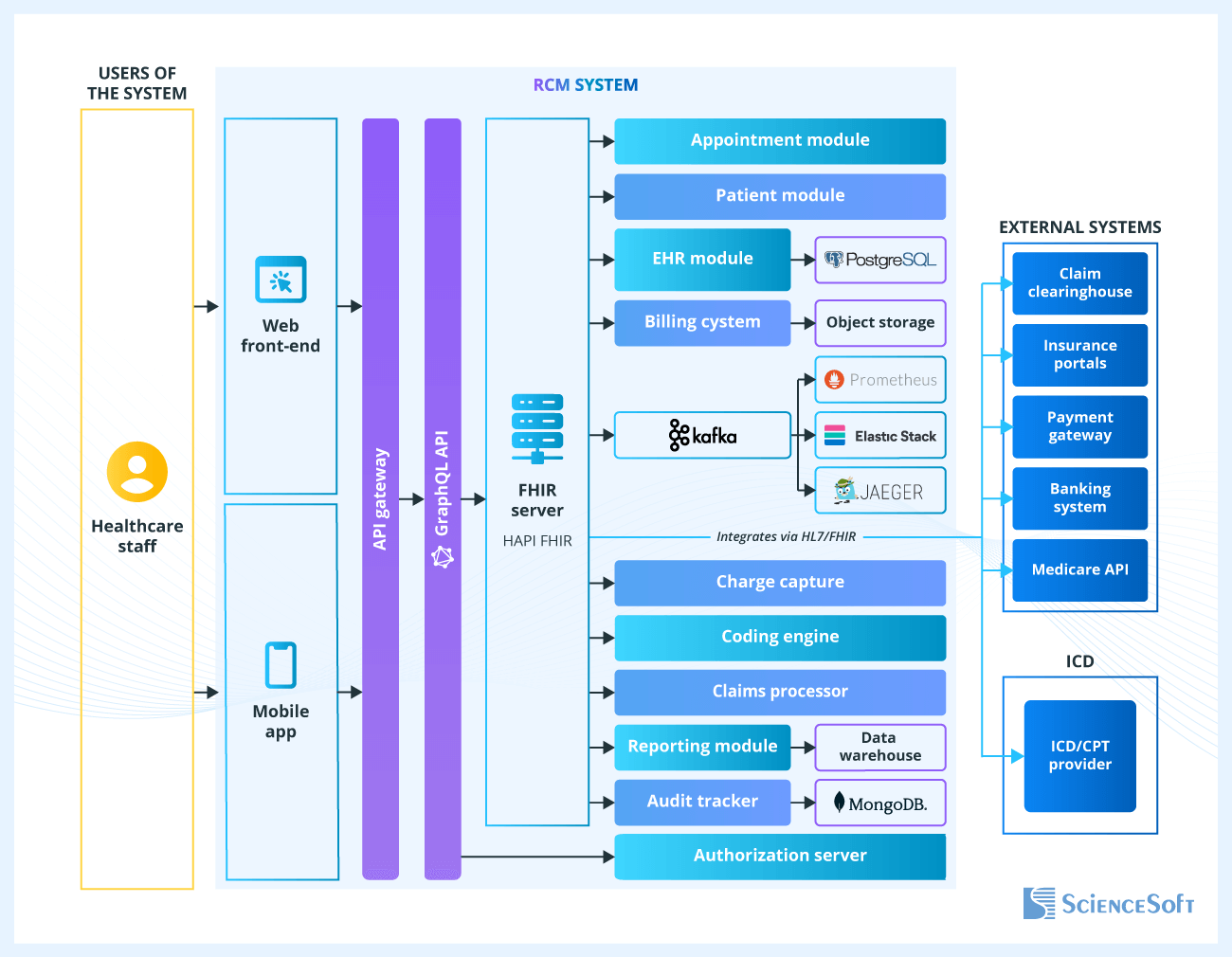
Healthcare staff interact with the software via mobile and desktop apps that utilize APIs and the FHIR server to request clinical and administrative data from corresponding modules. When data is pulled from certified EHRs, API payloads align to USCDI.
- The appointment module integrates with a clearinghouse to perform eligibility checks and request prior authorizations.
- The patient module interacts with the provider’s EHR to collect demographic and clinical data, and with the billing system to route self-pay information to a payment gateway and claims data to the clearinghouse.
- The charge capture module collects clinical service information for billing and feeds it into the billing engine.
- The patient billing system creates patient invoices, reconciles payments via external gateways (e.g., Stripe, InstaMed), and supports refunds, payment plans, and billing transparency via itemized receipts.
- The coding engine uses Medicare APIs to streamline coding procedures (e.g., suggest relevant codes, pinpoint compliance issues).
- The claims processing system generates and submits insurance claims using standardized code sets (e.g., ICD-10, CPT, HCPCS) and HIPAA X12 837/835 EDI transactions, tracks claim statuses, reconciles payments using ERA/EOB, and handles denials and resubmissions.
- The reporting module provides global revenue cycle analytics by aggregating claims and patient payment data flows into a shared view.
- An audit tracker logs all system interactions for compliance purposes.
- The authorization service is responsible for managing user access rights and enforcing security policies.
Custom RCM Software Development: Key Steps
Custom revenue cycle management development may be required to accommodate unique RCM workflows and revenue models (e.g., multi-entity operations, usage-based pricing, hybrid models with multiple revenue streams) and integrate diverse systems that lack native compatibility. A custom solution can also be more cost-efficient in the long run as it can help avoid subscription, licensing, and transaction fees typically charged by RCM software providers.
1.
Business analysis and requirements engineering
At this stage, healthcare software consultants communicate with the stakeholders (e.g., project managers, CIO, CFO, revenue cycle managers, billing and coding specialists) to elicit functional and non-functional requirements for the future RCM solution. They may need to gather information on the stages of the current RCM process, common errors and bottlenecks, and other software systems in use. The analysts also plan features that will support compliance with relevant regulations (e.g., data encryption at rest and in transit to comply with HIPAA, GDPR, and other data protection standards; GAAP and non-GAAP report generation to comply with ASC 606).
2.
Technical design
At this step, solution architects plan software modules that will support the required capabilities (e.g., workflow and rule engines to automate business processes, databases for patient, claim, and billing data). Architects also compare available technologies and suggest options that will ensure optimal performance, scalability, and elasticity at a reasonable cost. They also define integration approaches to connect the RCM with required systems (e.g., via standards like FHIR and HL7, or REST APIs). Where relevant, the design follows the 21st Century Cures Act interoperability provisions.
3.
UX/UI design
UX and UI designers create workflows and visual elements that would minimize the learning curve and make the solution easy to use. Designers may implement floating action buttons for frequent actions such as claim submission, use pre-filled fields to minimize errors, or prepare customizable dashboards for different user roles. If a mobile version of RCM is planned, UI designers will work on creating simplified interfaces that would be convenient to use on small screens.
One of the best UX/UI design practices we follow at ScienceSoft is auditing the client’s existing software and reusing familiar visual elements in the new solution. For RCM software, we may need to study existing financial management systems or EHR/EMR solutions in place. We may borrow hierarchical menus or sidebars, data input fields, and brand book styles. All this helps users feel “at home” in the app and adopt it faster.
4.
Development and testing
Developers build the solution’s back end and integrate it with the required systems. To speed up the process and reduce the risk of errors, engineers may go for feasible development automation practices (e.g., CI/CD implementation or low-code development). QA engineers perform usability, performance, and security testing and implement QA automation when possible. It’s a good practice for development and QA teams to work in parallel, which helps detect and fix issues early on.
5.
Deployment and support
The solution is deployed and monitored in a controlled environment. Developers control RCM solution performance and fix any remaining flaws. The team also prepares software maintenance guides for IT teams and educational materials for software users, including software manuals.
How Much Does It Cost to Develop Custom Revenue Cycle Management Software?
The cost of custom RCM software development may range from $500,000 to $2,500,000+. The primary cost factors include the number and complexity of solution features (e.g., rule-based or AI-powered analytics, batch or real-time data updates), the level of automation, and the difficulty of integrating the software with other systems.
$500,000—$1,500,000
Core RCM solution
Key capabilities:
- Integration with the core back-office systems like EHR/EMR.
- Batch and real-time data processing.
- Eligibility and insurance verification checks.
- Rule-based and automated charge capture and coding.
- Claim scrubbing tools.
- Claim submission and denial management.
- Basic revenue recognition methods, e.g., basis or simple accrual accounting.
- Core analytics and reporting capabilities, including KPI tracking, root cause analysis, and forecasting.
- Processing of up to 500,000 revenue transactions per month.
$1,500,000—$2,500,000
Advanced RCM solution
Capabilities of the core solution, plus:
- Extensive integrations depending on the provider’s needs, including with clearinghouses, payor systems, patient portals and apps.
- Automated prior authorization.
- AI-powered mechanisms that adjust charge capture forms based on past results.
- Real-time, automated reconciliation and complex revenue recognition methods, e.g., accrual accounting and percentage-of-completion.
- Advanced analytics capabilities, e.g., financial modeling.
- ML- and AI-powered mechanisms for insurance fraud detection.
- Processing over 1,000,000 revenue transactions per month.
Why Build Your RCM Software With ScienceSoft
- Since 2005 in custom healthcare software development.
- 150+ successful projects in the domain.
- Since 1989 in AI and machine learning.
- Experience in achieving compliance with data protection regulations (HIPAA, GDPR, PDPL, and PIPEDA), interoperability requirements (21st Century Cures Act), accounting standards (ASC 606, IFRS 15), and more.
- Proficiency with data exchange standards (e.g., (e.g., FHIR, HL7, DICOM, HIPAA ANSI X12 837 and 835) and coding systems (e.g., CPT, ICD-10).
Our awards, recognitions, and certifications
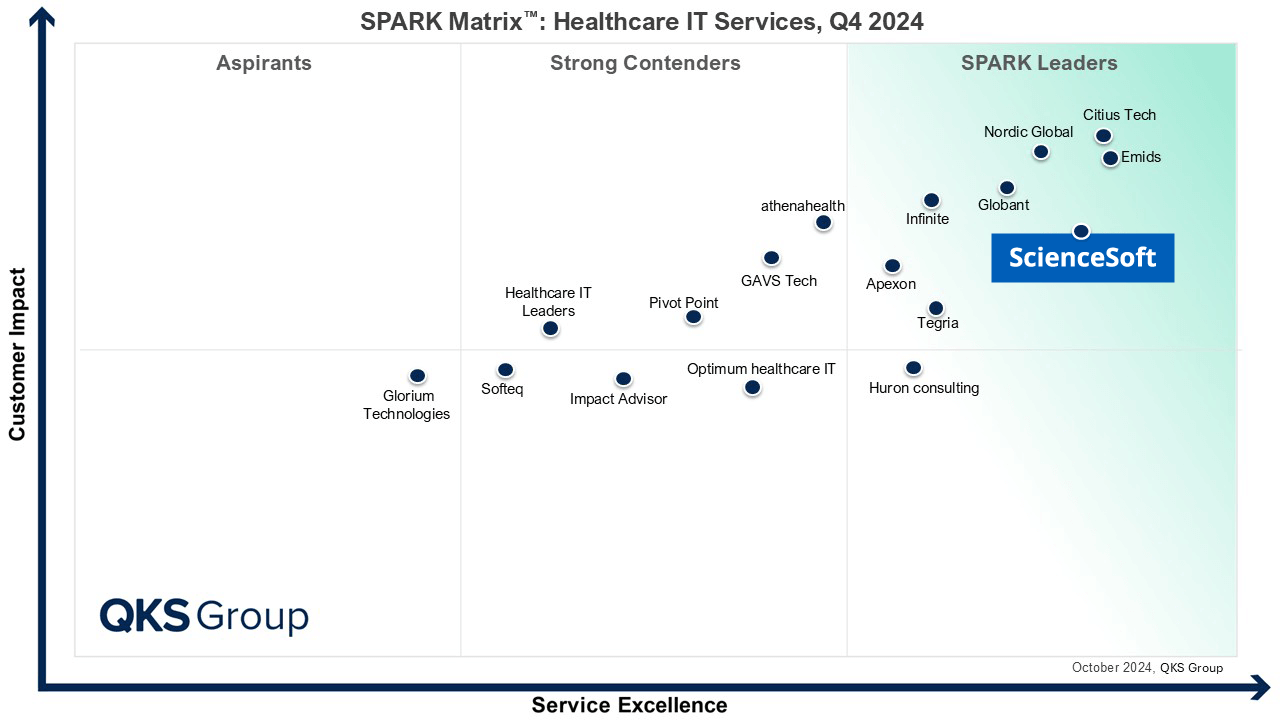
Featured among Healthcare IT Services Leaders in the 2022 and 2024 SPARK Matrix
Recognized for Healthcare Technology Leadership by Frost & Sullivan in 2023 and 2025
Named among America’s Fastest-Growing Companies by Financial Times, 4 years in a row
Top Healthcare IT Developer and Advisor by Black Book™ survey 2023
Four-time finalist across HTN Awards programs

Named to The Healthcare Technology Report’s Top 25 Healthcare Software Companies of 2025

HIMSS Gold member advancing digital healthcare
ISO 13485-certified quality management system
ISO 27001-certified security management system


