How Wearable Devices Support Efficient Health Monitoring
A wearable-based physiotherapy platform delivered by ScienceSoft led to a 70% reduction in pain and unnecessary surgeries among its users. Our clients get systems that drive measurable improvements in patient outcomes.
Wearable Health Monitoring Technology in a Nutshell
Wearable medical technology is increasingly used for health monitoring, chronic disease management, and preventive care. According to statistics, nearly 60% of US patients own a wearable healthcare device. These compact devices collect real-time physiological and behavioral data to provide clinicians with timely, actionable insights into the patients’ health trends.
Custom software for wearable-based health monitoring enables aligning the data capture and processing mechanisms with specific clinical needs. For example, in one of our projects, ScienceSoft’s team built custom motion capture algorithms to measure the range of motion of patient joints. The new algorithms significantly improved the accuracy and stability of the ROM sensors.
Wearable Device Market Overview
The wearable medical device market was valued at $42.74 billion in 2024 and projected to reach $168.29 billion in 2030, growing at a CAGR of 25.53%. The driving factors behind this growth include the rise of remote patient monitoring, the increasing demand for home healthcare, and a greater emphasis on a healthy lifestyle.
Sample Wearable Device Network Architecture
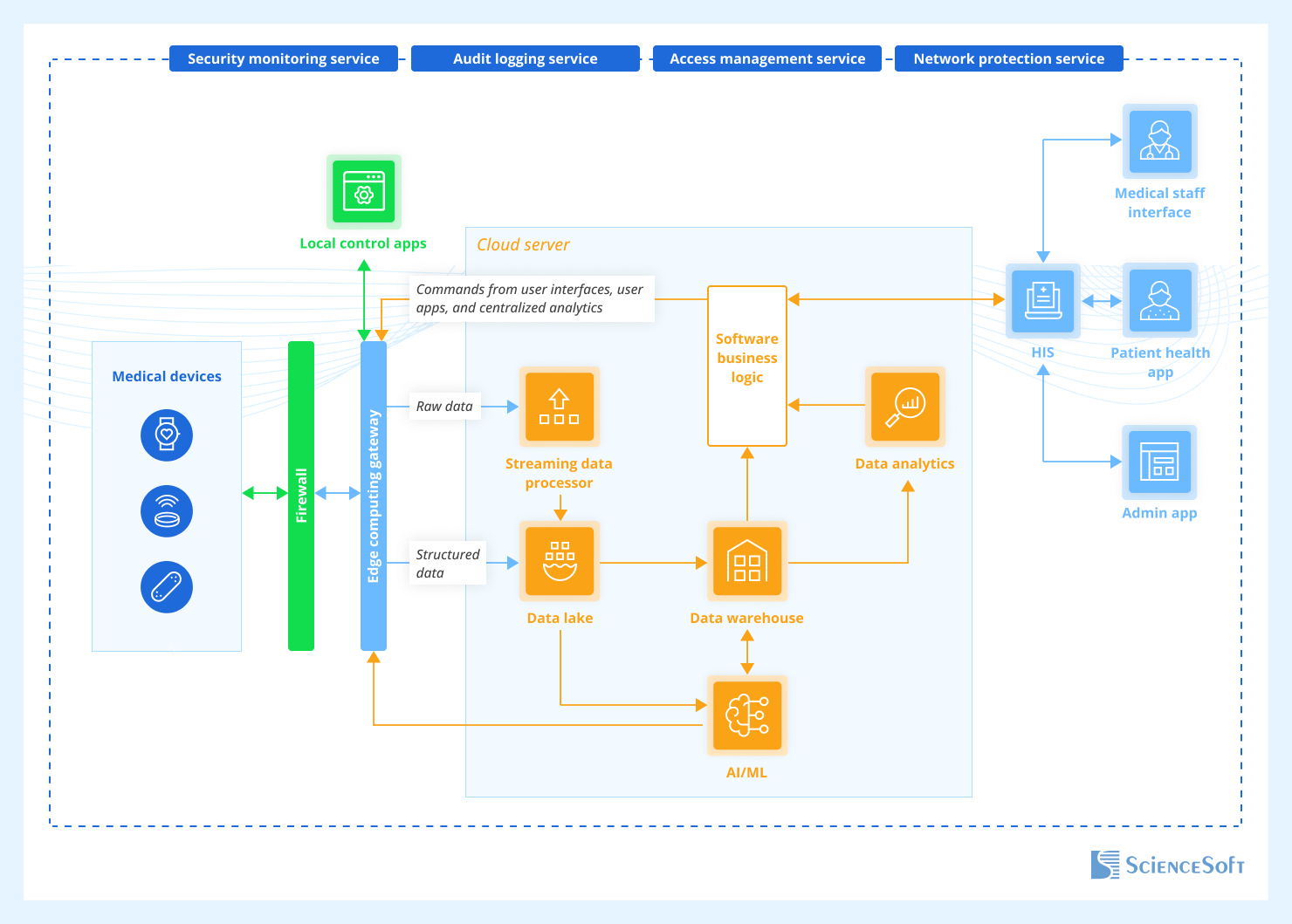
- Connected wearable devices transmit captured patient health information to the cloud back end via an edge gateway and firewall. The gateway temporarily stores the data (e.g., until a connection to a cloud is restored), filters redundant data, performs lightweight analytics, and forwards user commands (e.g., sampling frequency adjustments) from user apps to the devices.
- In the cloud, the stream processing module receives incoming data, analyzes it in real time, and enables low-latency responses such as alerts for abnormal health parameters. Raw and semi-structured data goes to the data lake, where it’s stored in its original format. After the data is cleaned and structured, it is sent to the data warehouse, where it’s available for fast querying, analytics, and reporting. The AI/ML engine processes raw data to enable the analytics module to detect anomalies in health data, predict health outcomes, or produce other high-level insights. Based on these insights, the engine can suggest or even directly perform setting adjustments via the edge gateway. Software business logic coordinates the workflows and routes relevant data between the system components (e.g., shows analytics results on the clinician’s dashboard).
- At the user interaction layer, role-specific interfaces connect to the back end via integrated hospital information systems (e.g., EHR, LIS, RIS), enabling clinicians and administrators to view relevant data and control device settings. Patients can also use dedicated apps to get limited insights into their health state and exchange messages with providers. The integrated systems also contribute contextual patient data, such as diagnoses, lab results, or medication history, to the cloud backend for more accurate analytics and decision-making.
- The entire ecosystem is safeguarded by dedicated services for access management, audit logging, threat monitoring, and network protection.
When discussing security in digital healthcare, access controls are often centered around people: who can access what, and when. But my experience shows that managing access at the device level is just as critical and often overlooked. Strong device identity verification allows healthcare organizations to ensure that only authorized devices can connect to the system and that all data comes from validated sources.
Common Application Areas and Capabilities of Wearable Health Monitoring Devices
Healthcare Providers Successfully Implementing Wearable Devices
Ochsner Health System launched a remote digital medicine program that used health monitoring devices like blood pressure cuffs and glucose monitors to help patients better manage hypertension and diabetes. The devices continuously measure patients’ blood pressure and blood sugar levels, and then automatically transmit this data to the Epic MyChart app and the EHR. Physicians then use the gathered data to personalize care plans. As a result, 79% of patients achieved better blood pressure control within 180 days. In the Digital Diabetes program, patients experienced a 57% reduction in hyperglycemia and a 74% reduction in hypoglycemic episodes, while 73% of patients from the control group showed no change in these measures.
Kaiser Permanente, in collaboration with Samsung, developed patient-facing mobile applications linked to Samsung smartwatches to deliver cardiac rehabilitation outside traditional rehabilitation centers. This approach relied on wearables to help patients monitor their activity levels and treatment progress, thus encouraging treatment adherence. The program achieved an 87% patient completion rate, representing a 74% improvement over traditional center-based rehab programs. Consequently, hospital readmission rates for cardiac rehab patients dropped to less than 2%.
Technologies We Use to Build Medical Device Networks
Device connectivity
Cloud services
Real-time data streaming

Data lakes
Tackling the Challenges Associated With Wearable IoMT
Cloud dependency risks
According to research, the cloud segment of IoMT is expected to experience the biggest growth from 2025 to 2030. Those aspiring to join the trend or maintain a competitive edge need a smart approach to implementing cloud connectivity in their solutions. If a medical wearable device relies too heavily on a cloud connection, it can lead to data loss, delayed alerts, and disruptions in health monitoring.
Solution
Data management optimization
Wearable devices must constantly capture large amounts of patient health data. If the management of this data is poorly organized, it can lead to unnecessary data transmission costs, increased power consumption, and delays in system performance.
Solution
Why Develop Software for Wearable Health Monitoring with ScienceSoft
- Since 2011 in IoT.
- Since 2005 in medical software engineering.
- 550+ developers. 50% of developers are seniors or leads with 9–20 years of experience.
- Experience in developing software compliant with HIPAA, HITECH, the Cures Act, GDPR, FDA, FTC, EU MDR requirements, etc.
- Proficiency in healthcare standards (e.g., HL7, FHIR, USCDI, SNOMED CT, LOINC, XDS/XDS-I).
- An official partner of Microsoft and AWS.
Our awards, recognitions, and certifications
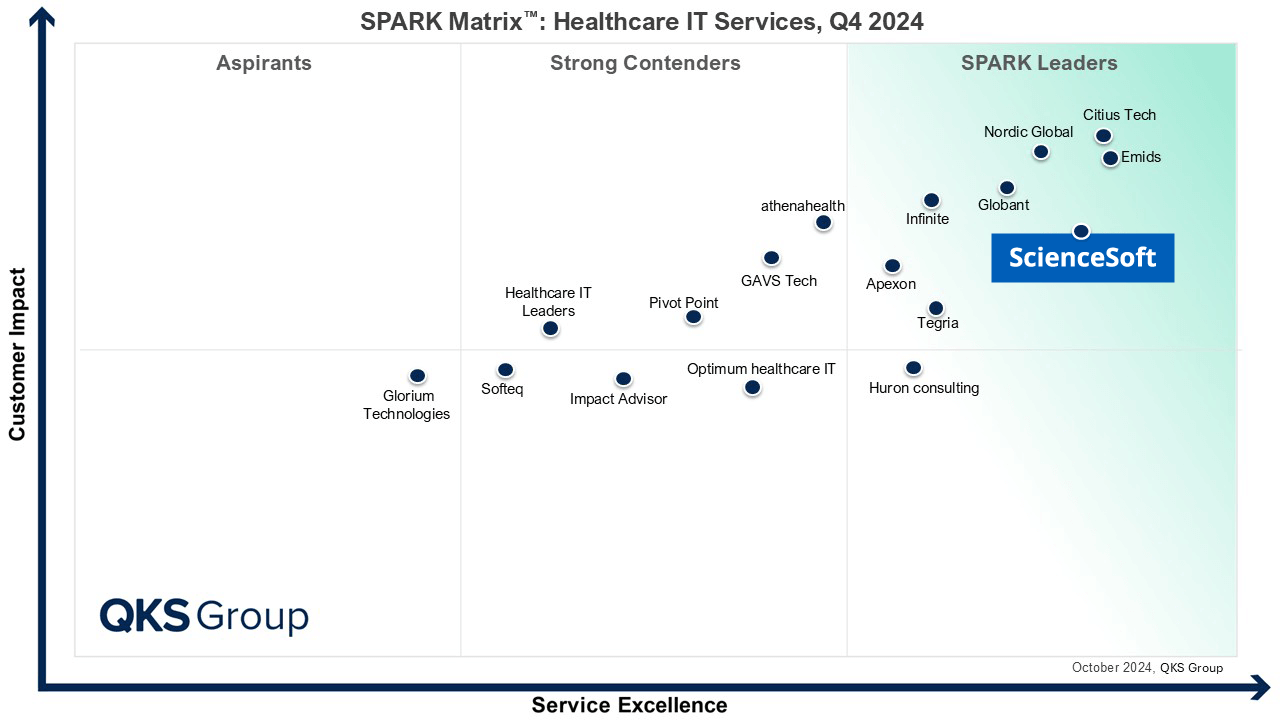
Featured among Healthcare IT Services Leaders in the 2022 and 2024 SPARK Matrix
Recognized for Healthcare Technology Leadership by Frost & Sullivan in 2023 and 2025
Named among America’s Fastest-Growing Companies by Financial Times, 4 years in a row
Top Healthcare IT Developer and Advisor by Black Book™ survey 2023
Four-time finalist across HTN Awards programs

Named to The Healthcare Technology Report’s Top 25 Healthcare Software Companies of 2025

HIMSS Gold member advancing digital healthcare
ISO 13485-certified quality management system
ISO 27001-certified security management system
How Much Does It Cost to Enable Wearable-Based Health Monitoring?
The costs of implementing wearable-based health monitoring technology typically range from $50,000 to $400,000+, depending on the following factors:
- Functional scope (e.g., the presence of advanced AI/ML-powered capabilities).
- Number and complexity of device integrations.
- Need for real-time data synchronization.
- Compliance requirements (e.g., the need for FDA submission).
- Development approach (e.g., native vs. cross-platform mobile apps, the need for a web app).
- Non-functional requirements (e.g., security, performance).
- Uniqueness of UX/UI design.
$50,000–$150,000
For a basic non-clinical fitness app that offers manual activity logging, GPS tracking, and a library of training and educational resources.
$200,000–$300,000
For a complex (but still non-clinical) fitness app that supports gamified progress-tracking and workout personalization based on each user’s goals and preferences.
$200,000–$400,000+
For EHR-integrated wearable-based remote patient monitoring software that can be augmented with clinical decision support and telemedicine capabilities.