EHR for Urgent Care
Capabilities, Integrations, Costs
In healthcare software engineering since 2005, ScienceSoft builds EHR systems for urgent care that speed up walk-in visits, tighten handoffs, and improve collections. We implement integration‑first solutions for hospital‑affiliated sites and all‑in‑one platforms for independent centers, always mapped to your patient volumes, staffing model, and partner ecosystem.
EHR for Urgent Care in Brief
An urgent care EHR is more than a generic EMR system. It's an operating platform covering urgent care workflows end-to-end from check‑in, live waitlist, triage, and single‑screen charting to order panels, e‑prescribing, revenue cycle automation, and visit summaries.
ScienceSoft implements custom urgent care EHR solutions for:
- Hospital‑tied urgent care sites where the urgent care module plugs into the hospital's other systems (generic EHR, RCM, LIS, RIS/PACS, billing, patient portals, etc.).
- Independent urgent care centers that require a specialized EHR to include all core workflows (check‑in, charting, X‑ray, billing, etc.), and integrate with reference labs and a clearinghouse.
Implementation time: from 12–24 weeks for a single‑site MVP.
Development costs: $250,000–$600,000+ for an integration-first MVP module for a hospital-tied urgent care site; $600,000–$1,200,000+ for a full-scale standalone platform with built-in modules for labs, imaging, billing, BI, and a patient portal. Use our free online calculator to get a tailored quote from our consultants.
Key Features of EMR for Urgent Care
Below you will find an outline of essential and advanced software capabilities most frequently requested by ScienceSoft's clients in urgent care. We tailor each solution's scope to the client's specific needs and workflows.
Core features
Value-adding features for urgent care EHR
Essential Integrations for Urgent Care EHR
To enable automated data exchange, ScienceSoft recommends building integrations on the following industry standards:
View data integration standards for urgent care EHR
Patient access and telehealth
- FHIR Appointment / HL7 SIU for scheduling, waitlists, and reminders.
- FHIR DocumentReference / CarePlan for after-visit summaries, discharge instructions.
- FHIR QuestionnaireResponse / Consent for eCheck-in, forms, patient consent.
- FHIR Encounter / Observation / DiagnosticReport for telehealth notes, observations, and reports.
Point-of-care devices & diagnostics
- HL7 ORU / IEEE 11073 for vitals and device results.
- HL7 ORM / ORU for POCT analyzer orders and results.
Imaging & radiology
- DICOM Modality Worklist for imaging worklists.
- DICOM/DICOMweb (QIDO/WADO/STOW) for image queries, retrieval, and storage.
- HL7 ORU / FHIR DiagnosticReport for teleradiology final reports.
Medications
- NCPDP SCRIPT 2017071 / RxNorm / EPCS for E-prescribing, medication coding, controlled substances.
Enterprise Clinical Data Exchange
- HL7 v2 (ADT/ORM/ORU/DFT/VXU) for admissions, orders, results, billing, immunizations, and syndromic feeds.
- C-CDA CCD / FHIR R4 US Core for clinical summaries, care plans, HIE exchange.
Revenue & payments
- X12 (270/271, 837P, 276/277, 835) for eligibility, claims, claim status, and remittance advice.
Using these as the foundation, we can help you set up the following integrations and more, depending on your IT ecosystem's specifics.
Hide
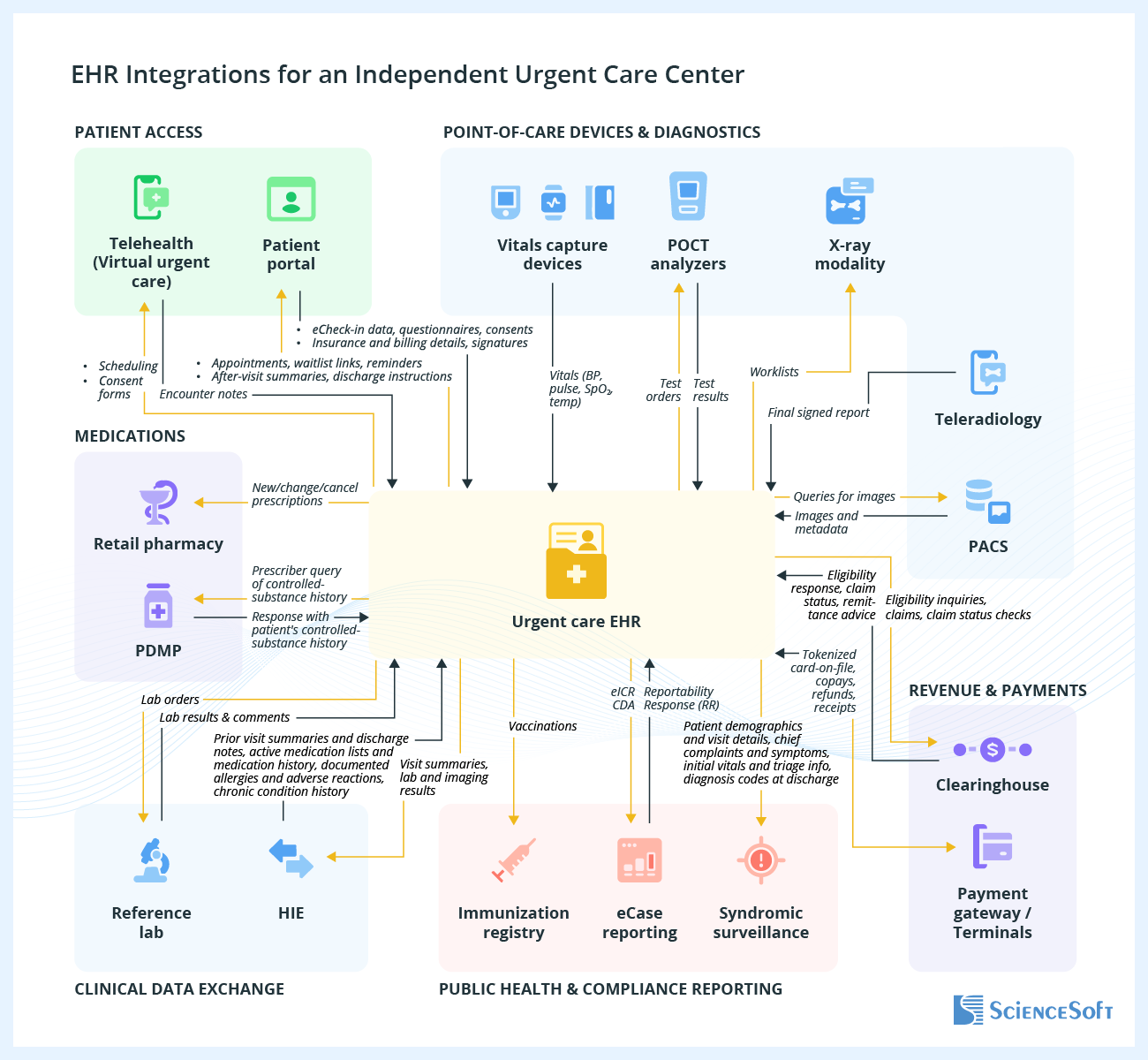
In the diagram above, we showcase potential integrations for an urgent care EHR of an independent urgent care center. In this setup, the center has its own portal, handles POCT in-house, sends other tests to a reference lab, operates an in-house X-ray with a separate PACS, uses a teleradiology and telehealth platform, and manages the full revenue cycle independently by sending claims to a clearinghouse. For a hospital-affiliated urgent care site, the integration architecture would include connections to the hospital's internal systems, including the enterprise EHR, LIS, RIS/PACS, billing/RCM, and patient portal.
A standalone urgent care EHR can exchange data with a patient portal (or the hospital's portal, if it's in place) so people can self-schedule or join a waitlist, complete eCheck-in, and receive AVS/discharge. It can also link with the tele-urgent care platform, so that scheduling and consent live in one place, and online visit notes come back into the record.
At the point of care, the system connects to vitals devices and POCT analyzers to pull readings and results straight into the chart. For imaging, it sends orders to the X-ray modality, requests images from PACS when they're ready, and ingests teleradiology reports so providers can review findings without leaving the EHR.
For medications, the EHR sends prescriptions to retail pharmacies (including EPCS for controlled drugs) and, where allowed, queries PDMP through a state-approved gateway once your organization is onboarded.
Clinical data can flow outward in two ways: independent centers typically connect to a reference lab and HIE to exchange summaries and results; hospital-affiliated sites swap those for the enterprise EHR/LIS/RIS-PACS, letting urgent care contribute to and draw from the hospital record instead of duplicating systems.
On the financial side, the EHR software for urgent care talks to a clearinghouse to automate eligibility, claims, status, and remits, and to a payment gateway/terminals for card-on-file, copays, refunds, and receipts. In hospital settings, charges can be handed off to enterprise RCM instead.
Public-health connections are added as needed: immunization reporting (with optional history/forecast), eCase Reporting, and syndromic feeds. These depend on jurisdictional onboarding and may go live on different timelines.
Key Steps of Urgent Care EHR Software Development
When building an EHR system tailored for urgent care workflows, ScienceSoft typically takes the following key steps:
1.
Discovery
ScienceSoft starts by meeting with urgent care stakeholders, such as the medical director, site manager, triage lead, and front-desk supervisor, to capture workflow gaps and improvement opportunities. Alongside that, we document measurable business objectives (e.g., reduce door-to-provider time below 20 minutes) and technical requirements (e.g., voice-enabled HPI and exam documentation) for the EHR. Our business analysts also gather input from future users like NPs, physicians, and X-ray technologists to define user roles and their tasks, and create accurate user personas. In parallel, compliance officers outline the applicable regulations and certifications (e.g., HIPAA, GDPR, 42 CFR Part 2, ONC, DEA EPCS, PDMP) that will shape system design. The outcome is a detailed Software Requirements Specification (SRS) that contains functional and non-functional requirements and sets the baseline for development.
Read more: ScienceSoft's Approach to Discovery in Software Development.
You usually need ONC certification only if your urgent care EHR is used for Medicare Promoting Interoperability (PI) or if a payer or partner specifically asks for it. Independent urgent care centers, or hospital departments that already use a certified enterprise EHR for core administration, normally don't need to certify their urgent care platforms. Still, it's best to build the system on HL7/FHIR standards so it connects easily with other software now and is ready for the future.
2.
Architecture design
Drawing on discovery results, solution architects build a secure and scalable blueprint for the urgent care platform. We typically recommend a modular (microservices/SOA) approach, which is best suited for complex healthcare solutions. Each service handles a specific function, for example, check-in, triage, charting, orders, e-prescribing, revenue cycle, or analytics. This approach ensures fast, reliable performance, while allowing individual components to be scaled, updated, or replaced independently without disrupting critical operations.
The deliverables of this stage include diagrams of system components, data flows, and integration points, as well as deployment guidance. Security and resilience patterns are embedded by design to ensure compliance with HIPAA, GDPR, and other applicable regulations.
Read more: ScienceSoft's Approach to Software Architecture Design.
Using an interface engine for integration is more reliable than creating many direct connections between systems. The engine manages data exchange: it converts formats (HL7 v2, FHIR, X12, NCPDP, Direct), checks quality, retries failed transfers, and monitors activity.
Hospital-affiliated urgent care sites can usually rely on the hospital's existing engines to connect to the hospital's systems, such as EHR/MPI, LIS, RIS/PACS, billing/RCM, portals, HIE, and public health systems. Independent centers benefit from a lightweight option to tie their EHR to POCT devices, reference labs, PACS/teleradiology, pharmacy/eRx/PDMP gateways, clearinghouses, payment gateways, immunization and case-reporting registries, and telehealth platforms.
This setup reduces integration risks, speeds up partner onboarding, and makes scaling to more sites easier.
3.
UX and UI design
ScienceSoft's design team prepares wireframes and clickable prototypes for urgent care interfaces, including online check-in, triage, complaint-based charting, and order entry. Prototypes are tested with staff (front desk, nurses, providers, X-ray technologists, and billing) using real cases like pediatric dosing, acute injury with imaging, strep testing with eRx, and occupational visits.
In urgent care, UX design emphasizes:
- Speed under pressure: large action buttons, predictable tab order, visible room status, and shortcuts for repetitive tasks.
- Patient safety: automated ED referral triggers, weight-based pediatric dose checks, PDMP/allergy/interaction reminders before prescribing, QC prompts for POCT, pregnancy alerts before imaging, and discharge defaults for return precautions.
- Multitasking support: multi-user charting, inline order sets, undo/redo, quick-switch between patients, and persistent panes for meds/allergies/results.
The result of this stage is an interactive prototype tailored to urgent care workflows and tested against real-life scenarios.
Read more: ScienceSoft's Approach to User Convenience in Healthcare Software, How ScienceSoft Designs Software UI.
4.
Development and testing
Urgent care solutions are built in stages, first rolling out a validated MVP covering tightly defined workflows (intake, triage, charting, orders, prescribing, and billing) and then extending it with larger feature updates. Development is split into increments mapped to clinical tasks (e.g., complaint-based charting, lab/X-ray ordering, eRx/EPCS, RCM), each with clear benchmarks such as median charting time ≤90 seconds, ≥99.5% result posting accuracy, and ≥92% clean claims.
ScienceSoft validates integrations through the interface engine (HL7, FHIR, X12, NCPDP/EPCS, Direct, DICOM/DICOMweb) to ensure correct routing, transformations, retries, and alerts.
Clinical safety checks cover urgent-care-specific risks like red-flag triage to ED, pediatric dose limits, allergy/interaction alerts, POCT QC, and discharge defaults, with compliance enforced for HIPAA, DEA EPCS, PCI-DSS, CLIA, SSO/RBAC, encryption, and DR/HA.
Read more: How ScienceSoft Approaches Software Development Projects.
5.
Pre-launch, deployment, and training
During pre-launch, ScienceSoft submissions to regulatory authorities (e.g., ONC), if required. We also prepare training packs and quick-start guides tailored to urgent care roles. Staff training is tailored to each role: front desk (eligibility and payments), triage nurses (intake, vitals, red-flag routing), and providers (express notes, one-click orders, eRx/EPCS). Training can be delivered on-site or virtually.
Go-live is staged with rollback options, followed by 2–4 weeks of KPI monitoring (door-to-provider, LOS, eligibility latency, clean-claim rate, callback closure) and fixes as needed.
Read more: How ScienceSoft Ensures Effective Knowledge Transfer and Training for Healthcare Software Users
How Much Does It Cost to Develop an EHR System for Urgent Care?
Key cost factors
Based on ScienceSoft's experience, the cost of building electronic health/medical records for urgent care varies significantly depending on the following factors:
- The number of sites that the system must handle.
- In-system lab test orders (higher investment) vs. integration with the existing LIS system.
- In-system imaging (higher investment) vs. integration with the existing RIS/PACS system.
- In-system billing (higher investment) vs. integration with the existing RCM system.
- Native patient app or portal (higher investment) vs. integration with the existing portal.
- Security and resilience requirements.
- The need to add assistive AI features, such as dictation engines.
- The need for ONC certification.
Learn the cost of your EHR platform
ScienceSoft's team is ready to provide a custom quote for your specific case.
Why Choose ScienceSoft as Your Urgent Care Software Development Partner
- Over 150 successful healthcare IT projects.
- In cybersecurity since 2003 to ensure reliable protection of software and IT environments holding PHI.
- 10 principal architects, each with 15+ years of experience designing enterprise-wide systems and proven expertise in complex and legacy healthcare integrations.
- Experience in achieving compliance with the requirements of HIPAA, GDPR, 42 CFR Part 2, CEHRT, and the 21st Century Cures Act.
- Deep knowledge of data exchange standards such as FHIR, XDS/XDS-I, C-CDA, and USCDI.
- Expertise in clinical coding and terminology standards such as ICD-10, CPT, SNOMED CT, LOINC, and RxNorm.
Our awards, recognitions, and certifications
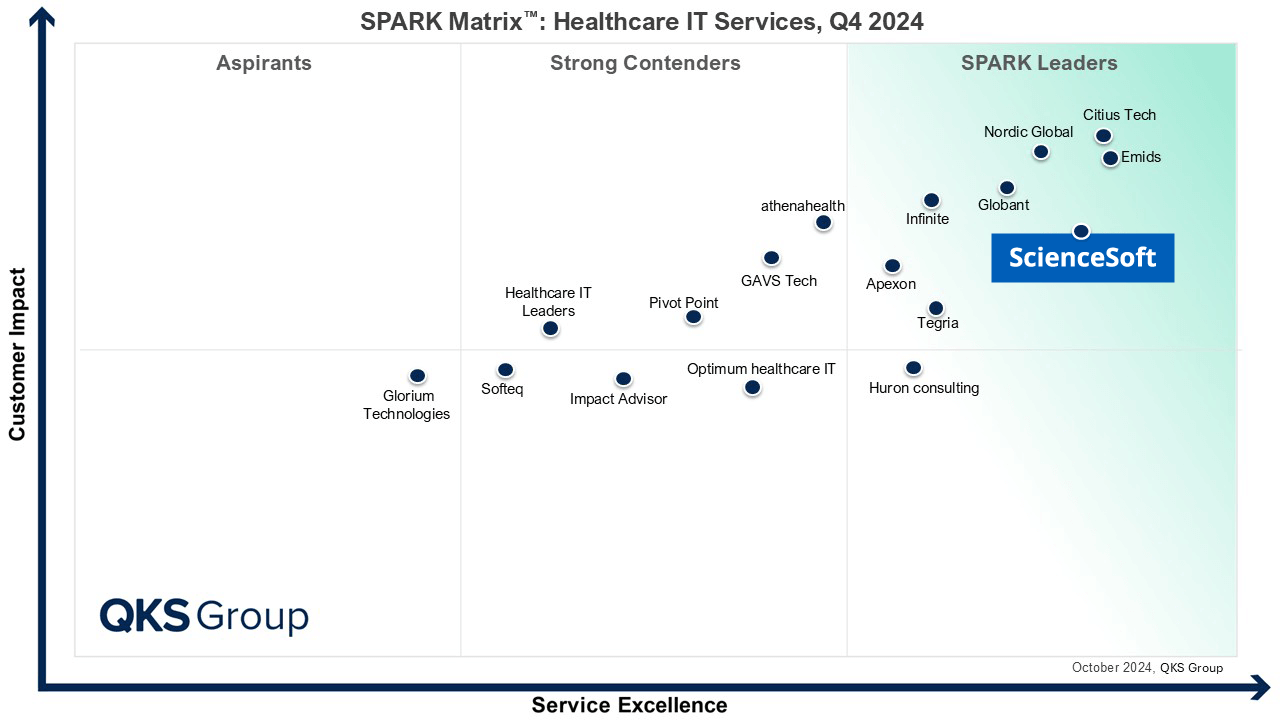
Featured among Healthcare IT Services Leaders in the 2022 and 2024 SPARK Matrix
Recognized for Healthcare Technology Leadership by Frost & Sullivan in 2023 and 2025
Named among America’s Fastest-Growing Companies by Financial Times, 4 years in a row
Top Healthcare IT Developer and Advisor by Black Book™ survey 2023
Four-time finalist across HTN Awards programs

Named to The Healthcare Technology Report’s Top 25 Healthcare Software Companies of 2025

HIMSS Gold member advancing digital healthcare
ISO 13485-certified quality management system
ISO 27001-certified security management system







