Healthcare Data Analytics
Software Solutions, Costs, Outcomes
Since 1989 in data analytics and since 2005 in healthcare IT, ScienceSoft builds custom and platform-based analytics software that streamlines clinical decision-making, optimizes operations and costs, and enables care personalization.
Healthcare Data Analytics: the Essence
Healthcare analytics is needed to consolidate and analyze multi-source data related to patient health, clinical processes, and healthcare business operations. Specialized healthcare analytics solutions help improve health outcomes, promote value-based care, support clinical decisioning, and achieve higher business process efficiency.
- Integrations: EHR/EMR, healthcare CRM, patient portals and apps, remote patient monitoring software, medical image analysis software, healthcare asset tracking software, and more.
- Implementation costs: $100,000–$1,250,000, depending on the number of integrated sources, data complexity, compliance requirements, AI/ML-powered analytics, and more. You are welcome to use our cost calculator to get a tailored ballpark estimate for your project.
- ROI: up to 350%.
Healthcare Analytics Software: Key Features
Below, ScienceSoft’s consultants list the key analytics software capabilities most requested by our clients in the healthcare domain.
General analytics features
Specific healthcare analytics features
Advanced AI & ML capabilities
Healthcare analytics solutions with advanced clinical decision support features may be classified as Software as a Medical Device (SaMD). For instance, this applies to software that enables remote control over wearable medical devices (e.g., an infusion pump or an implantable neuromuscular stimulator), provides AI-powered interpretation of medical images and test results, or sends alerts on patients’ states for potential clinical intervention. Since such software can directly affect patients and significantly influence treatment-related decisions, it must comply with IEC 62304:2006/Amd 1:2015 and ISO 13485 standards and requires FDA approval. To make sure our clients have flexibility in choosing their healthcare analytics features, ScienceSoft invests heavily in our expertise with the above regulations. We are ready to appoint relevant compliance experts to guarantee the future software adheres to all the requirements no matter how strict they are.
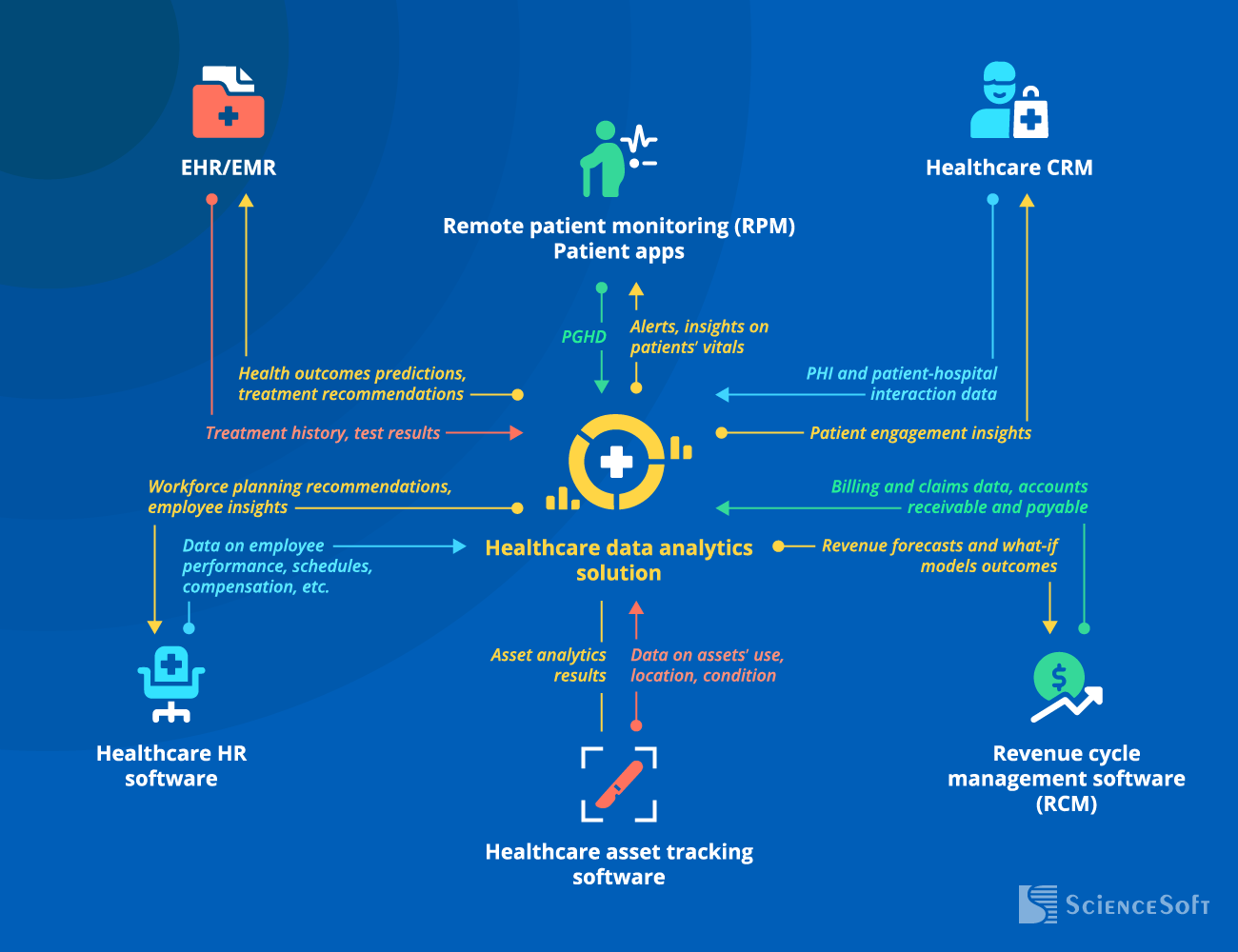
4 Types of Healthcare Analytics
When implementing healthcare analytics software, ScienceSoft differentiates between the following four types of analytics. Simpler systems may only enable one or two of them, while the most advanced solutions often combine all four.
Descriptive
Analyzes historical data to say what happened. For instance, to calculate the average ER wait time for the last month.
Diagnostic
Uses historical data and statistical analytics techniques to explain why things happened. For instance, why the average ER wait time was higher than usual last month.
Predictive
Applies AI/ML capabilities to historical data and builds what-if scenarios to predict what will happen. For instance, how high the average wait time will be next month.
Prescriptive
Uses AI/ML capabilities to recommend what to do to avoid an unfavorable prediction and achieve better results. For instance, how to reallocate stuff to avoid high ER wait times.
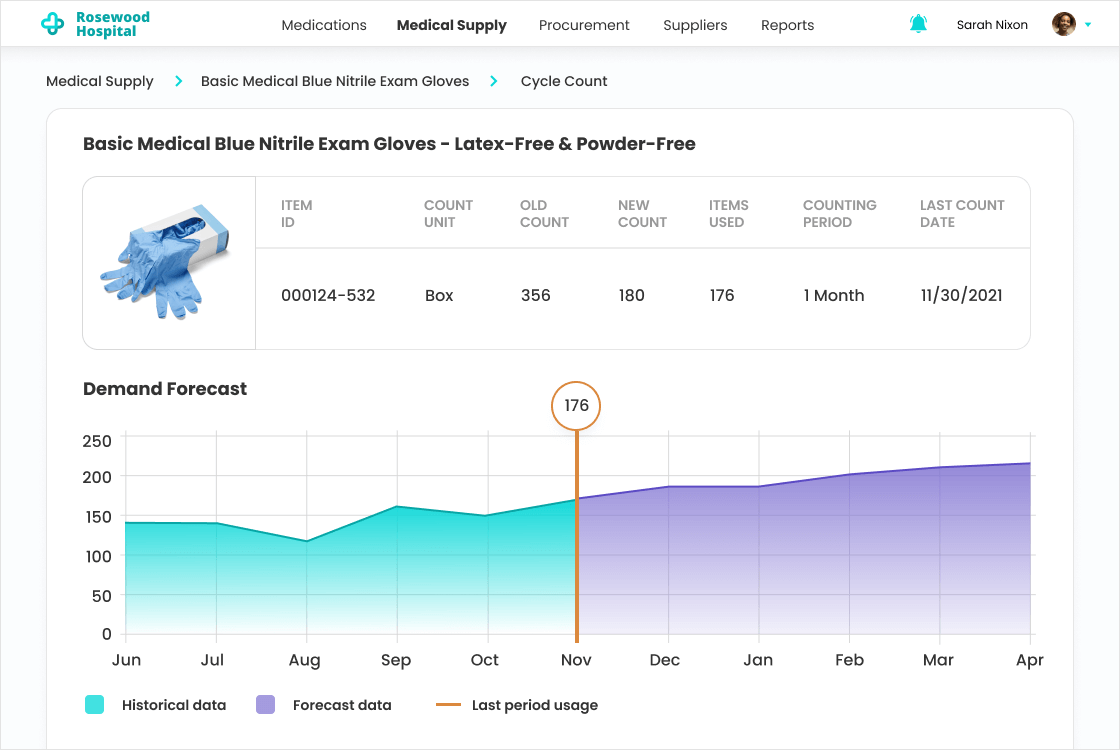
Essential Integrations for a Healthcare Data Analytics Solution
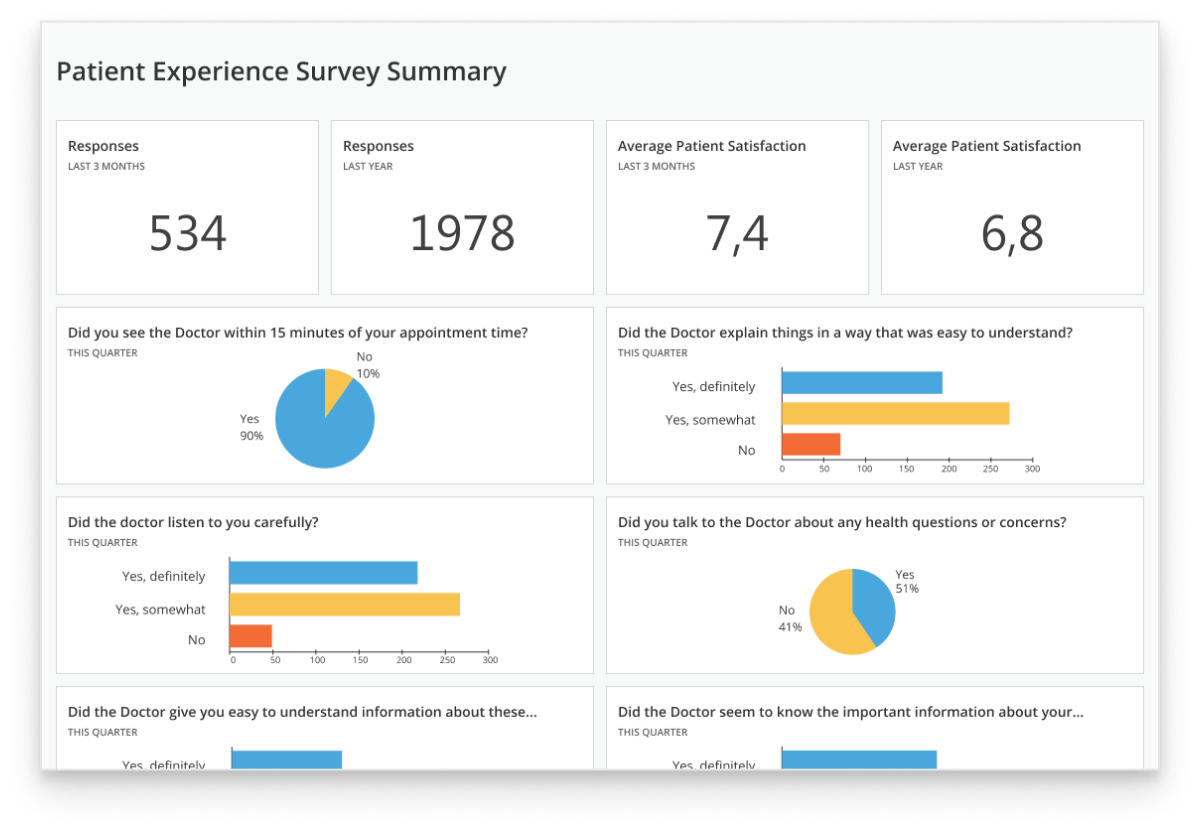
To support clinical decision-making (e.g., by facilitating diagnosing or suggesting the most effective treatment option).
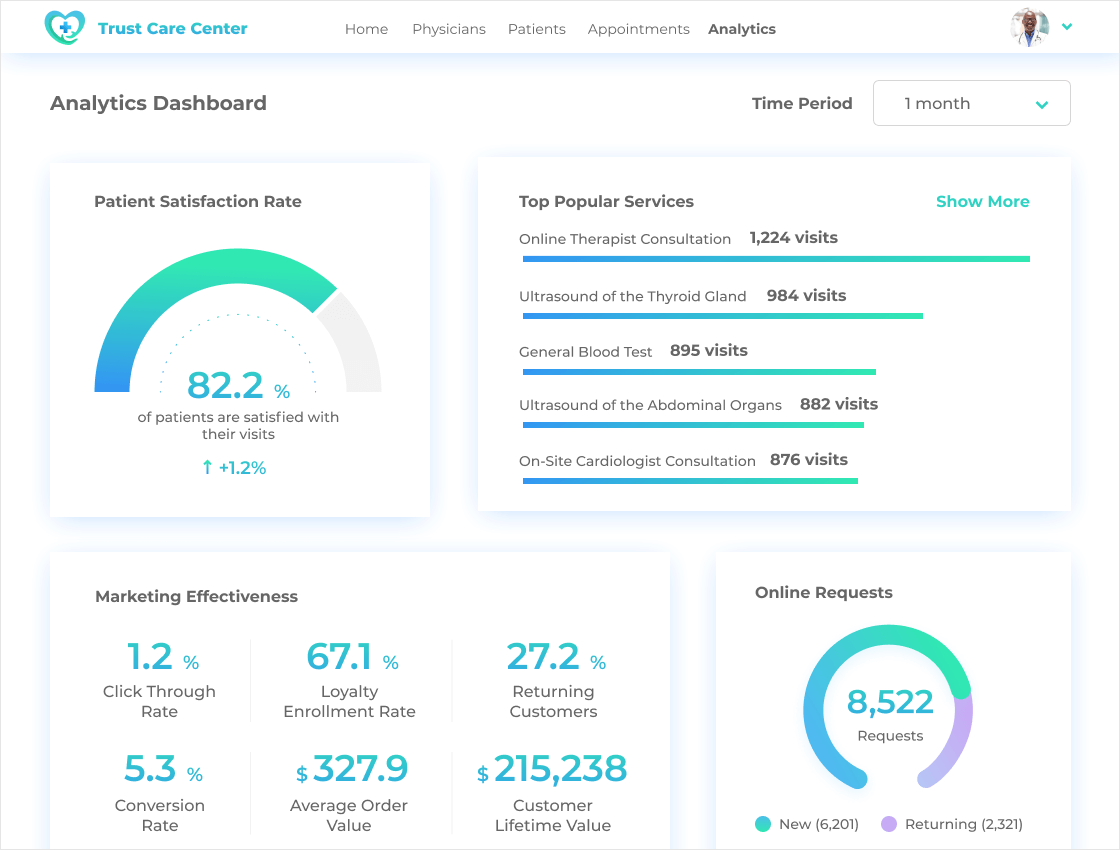
- To enable efficient patient segmentation and targeting.
- To identify best practices and service gaps.
Note: Alternatively, your healthcare analytics solution can be integrated with call center software.
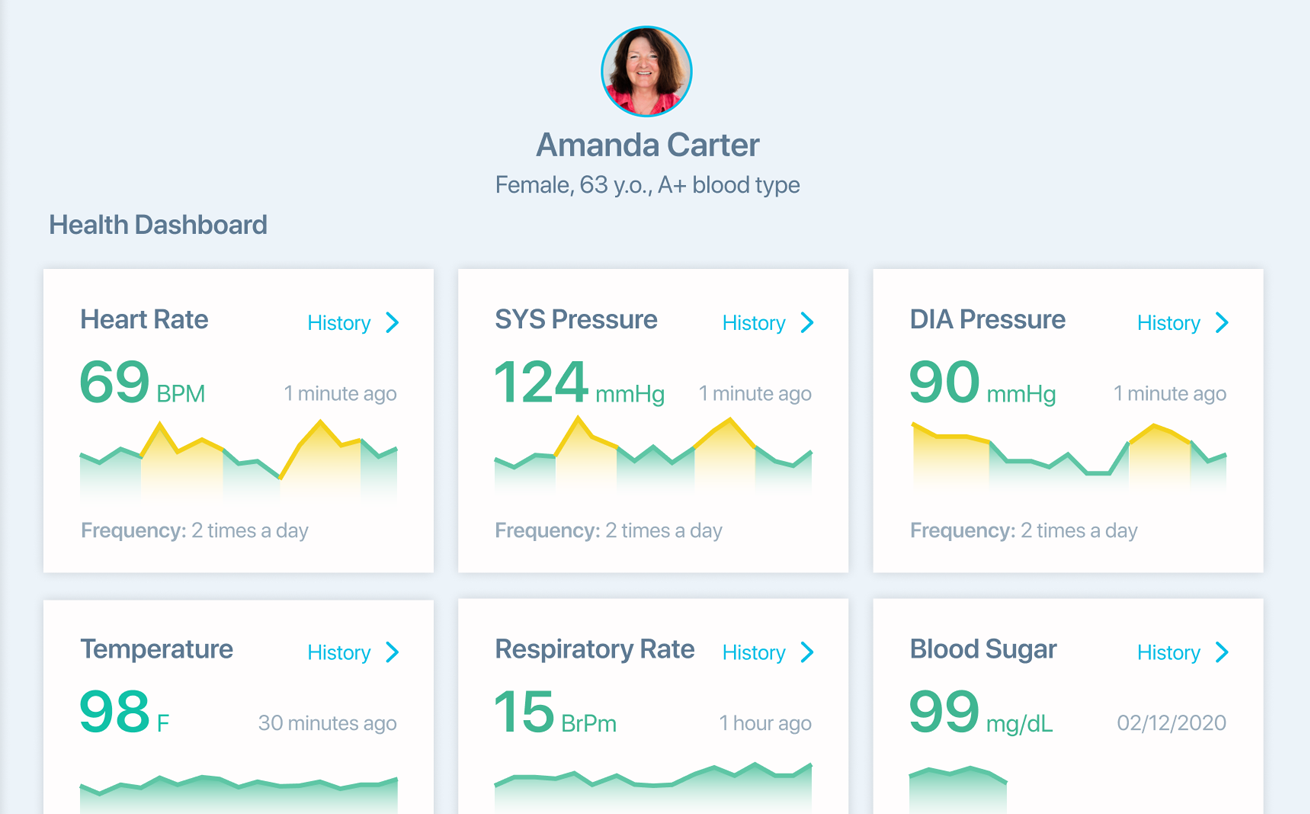
- To enable continuous monitoring and analytics of the patients’ vitals with immediate alerts in case of abnormal readings.
- To ensure personalized care or patient management depending on a particular condition or goal.
- To optimize employee engagement and retention strategies and ensure proper staff credentialing.
- To shape and improve initiatives for employee performance optimization.
- To ensure smooth scheduling.
- To enable billing and financial management optimization and increase revenue.
- To ensure automatic detection of fraudulent claims.
- To optimize asset utilization and minimize related losses (e.g., due to missed opportunities for reuse or incorrect storage conditions).
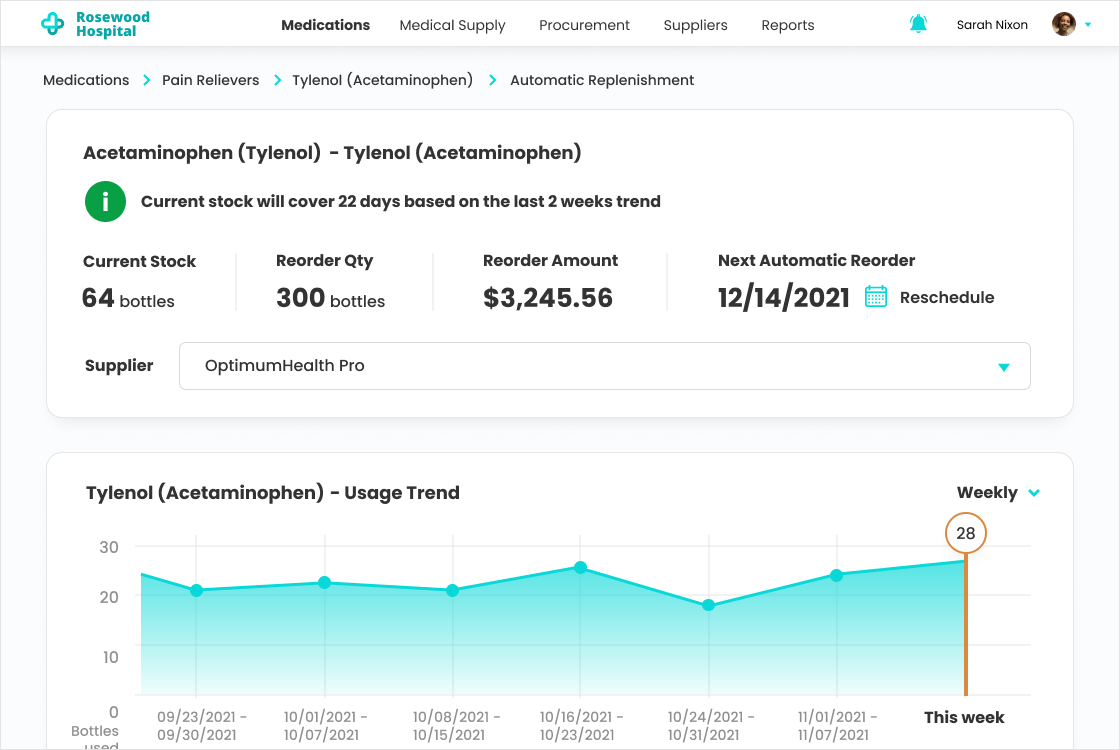
- To improve inventory management.
- To enable efficient medication distribution control and decrease medication shortage risks.
- To plan timely equipment maintenance.
Multiple EHR-adjacent software systems (e.g., practice management, LIS, HIE) can communicate with the analytics module via the integrated EHR or directly via APIs. In each specific case, we design a custom integration architecture based on our clients’ unique IT infrastructure to deliver the most efficient solution.
How ScienceSoft Drives Value of Healthcare Analytics Solutions
We follow our established practices for scoping, cost estimation, risk mitigation, and other project management aspects to reach project goals regardless of time, budget, and change request constraints.
Tailored functionality
With off-the-shelf software, you often have to settle for standard functions that don’t fit your processes, or pay for fancy features you don’t need. Focused on bringing value with our services, we plan and implement efficient software that answers the specific needs of our clients.
Mature Agile culture
Relying on mature Agile processes established over decades of practical experience, we can deliver an analytics system MVP in 2–6 months and gradually upgrade it to the fully-featured solution in stable 2–4-week iterations.
Cost optimization
To optimize software development costs, our developers use proven third-party components, open-source APIs, and microservices that enable significant code reuse. Our established DevOps practices, efficient CI/CD design, and feasible QA automation help us reduce the total development cost by up to 78%.
Focus on security and compliance
Proud of having zero security breaches in our 36-year history, we keep investing in our ISO 27001-certified security management system. With a team of in-house security engineers and regulatory consultants, including HIMSS-certified experts, we can guarantee full software compliance with HIPAA, GDPR, FDA requirements, and more.
Advanced technologies
In data science since 1989, we enhance analytics solutions with AI capabilities that power intelligent automation and forecasting. We also apply a decade of experience in big data to ensure accurate and timely analytics across massive data sets.
Costs and Benefits of Healthcare Data Analytics Implementation
The cost of healthcare analytics may vary from $100,000 to $1,250,000, depending on data complexity and diversity, the number of integrations, the presence of AI/ML analytics capabilities, and more.
$100,000–$250,000
A basic solution that:
- Integrates with 1-3 key data sources, like EHR or CRM.
- Enables batch data processing (e.g., once every 24 hours).
- Calculates the essential operational and financial KPIs.
- Identifies trends and dependencies in health and operational data.
$250,000–$500,000
A solution of medium complexity that:
- Integrates with multiple internal sources (e.g., RMS, asset tracking software, HR software).
- Enables batch and real-time analytics.
- Enables root-cause analysis, patient and outcomes segmentation, and forecasting.
- Provides rule-based and ML-powered analytics.
$500,000–$1,250,000
An advanced solution that:
- Integrates with any number of internal and external sources, including unlimited patient apps and IoT devices.
- Integrates with several same-type sources, e.g., two CRMs of different divisions.
- Enables batch and real-time analytics, including big data processing.
- Enables advanced analytics, including AI-powered predictions and recommendations.
Want a more precise figure?
Our consultants will provide a tailored cost estimate for your data analytics initiative.
*Software license fees are not included.
87% of Organizations Report Measurable Business Value from Their Data Analytics Investments
The 2024 Data and AI Leadership Executive Survey is based on feedback from over 100 global industry leaders that have implemented data analytics solutions. The report features 10+ prominent organizations from the healthcare domain, including Pfizer, Mayo Clinic, UCLA Health, and more.
Market-Available vs. Custom Healthcare Analytics Software
When searching for out-of-the-box solutions, you’ll find several platforms that offer ready-made products for different types of analytics (e.g., for patient outcomes, revenue cycle tracking). Although these products can be customized or integrated into one with the help of native APIs, the capabilities of such software are still limited to a predefined set of features. If you are looking for a comprehensive system covering several analytics types at once (e.g., finance, operations, asset tracking) or a highly precise tool for a medical specialty (e.g., CDS for oncology), you’re likely to find OOTB solutions insufficient.
On the other hand, custom software means you’re getting a tailored solution that meets all your analytics needs and fits your unique IT environment. The downsides of custom software are related to substantial initial investments and relatively lengthy implementation. However, such solutions drive up to 350% ROI with an average payback period of 9 months, which makes the investments worthwhile in the long run.
The high ROI of custom solutions is driven by:
- A bespoke feature set with any level of analytics complexity (e.g., multi-dimensional patient segmentation, financial analytics across different taxation systems).
- Smooth integration with all the required systems: back-office and legacy software, third-party platforms (e.g., a clearinghouse), IoT devices, and more.
- Compliance with the required global or local regulations (e.g., HIPAA, FDA, ADHICS), convenient functionality for compliance checks and reporting.
- Guaranteed scalability in case of user and data volume increase.
- Tailored interfaces for different user groups (e.g., hospital administrators, physicians, MLSs), leading to increased convenience and higher productivity.
Build Your Healthcare Data Analytics Solution with Experts
About ScienceSoft
ScienceSoft is an IT consulting and software development company headquartered in McKinney, Texas. Since 2005, we have been helping healthcare organizations leverage the potential of advanced data analytics to deliver better care, improve health outcomes, and achieve better operational efficiency. Our mission is to drive your project success in spite of time and budget constraints, as well as changing requirements. Being ISO 13485, ISO 9001, and ISO 27001-certified, we can guarantee top software quality and complete security of our clients’ data.