Tech-run chronic disease management model: when care providers do care
Even though most of chronic conditions are noncommunicable, the World Health Organization acknowledges their epidemic nature. Sadly, ‘epidemic’ is not an exaggeration.
Chronic disease initiatives going wrong
Chronic conditions are responsible for disabilities and 7 of 10 deaths each year.
Young or old, we are all in the same boat. Centers for Disease Control and Prevention (CDC) points out that 76.4% of all US adults (194 million people) had one or more chronic conditions as of 2023 (the latest available data). “As the US population ages, and people live longer, the number of people with multiple chronic conditions is expected to continue to grow”, states AHRQ.
It’s no secret that great efforts are put into the management of long-term conditions. Yet, a lot of such initiatives are on the wrong track, and it takes just a glance at statistics on complications to prove that. For example:
- 80% of adults with disabilities have at least one chronic condition.
- According to the CDC, diabetes is the No. 1 cause of kidney failure, lower-limb amputations, and adult blindness.
Overall, these statistics show that there is no significant improvement in chronic disease treatment and management so far.
How technology helps
As chronic conditions directly affect almost half of the nation, the chances of developing one at some point in life are rather high. They lower the quality of life, put patients into emergency rooms and hospital beds, cause disabilities, and premature deaths. However, even when it’s impossible to wipe out the conditions themselves, there is a high potential to reduce their negative health outcomes with the help of chronic disease management software.
Practically, it should help both care providers and patients achieve 3 extremely important goals:
- Reduced chances of developing complications and comorbidities
- Reduced preventable readmissions
- Improved life quality of patients
Looking at the numbers above, it’s clear that current activities lack something that can back up reaching these objectives.
This something is the alliance of systematic care and patient engagement, apparently troublesome to create in today’s healthcare environment. However, technology is able to resolve this issue. Not just any technology, of course.
We see the tech-run chronic disease management model as an equation of the following components:
Healthcare CRM + Patient Mobile App + Patient-Generated Health Data (PGHD)
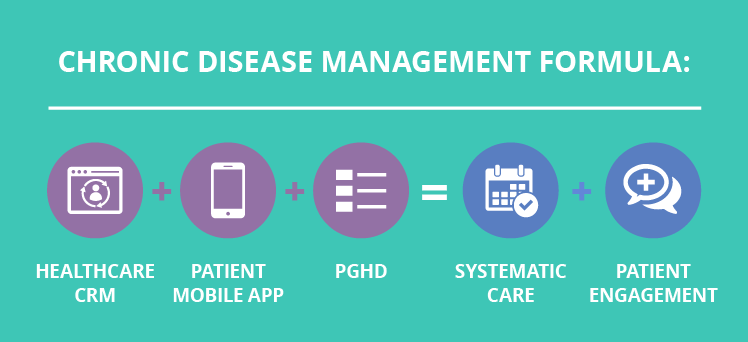
This equation has a real potential to transform current chronic care delivery with all its gaps and loopholes into the system that will actually work for the benefit of both patients and healthcare providers. Let's dive deeper and find the proofs.
Cornerstones of tech-run chronic condition management
It takes two to succeed in keeping the long-term disease under control: systematic care and patient engagement. Without them, care providers can’t guarantee full understanding of the condition’s history and progress, relevant treatment plan, and effective prevention of complications. Patients, from their side, tend to fall into depression, give up on their condition management, mistreat their symptoms, skip scheduled appointments, and procedures.
Why is technology a driver here? Simply because there is no practical way to support systematic care and patient engagement effectively without tech-based tools. Considering patients' life quality, it is impossible to establish continuous care by putting all individuals in hospital beds for the rest of their lives. Especially since there are 194+ million of them.
Patient engagement is also a hard nut to crack without any tech-based tools, as providers can’t call their patients to ask what is going on, to remind them to take pills, to behave and eat healthily.
Thus, we encourage you to take a look at how our equation delicately yet firmly supports both systematic care and patient engagement.
Systematic care: problems and solutions
As we already discovered, the main problem with continuous care is that there is none.
In the long-term prospect, some patients visit their doctor once a month, and some show up once in a few quarters or even years. In this situation, even care delivery itself is questionable, not to mention its consistency. Not blaming either patients or physicians, this is not how chronic conditions should be managed.
Individuals tend to forget about appointments and completely give up on them in a couple of months. Then they skip necessary checks and lab tests, don’t get accurate treatment plan updates, and find themselves in the emergency room with acute complications (not even in the worst-case scenario). When patients are stabilized, they are still left without comprehensive guidelines on their condition management, so this pattern keeps repeating.
Physicians, in turn, provide patients with primary information, but they can’t dive into details and pack all the necessary knowledge into a 15-minute appointment. So they say their goodbyes and hope an individual either will come back for more information or search for necessary guidelines online and succeed in self-management. What happens after a patient leaves the clinic after an appointment or even a hospital after treating complications? Their physician doesn’t know.
Accordingly, a whole range of current chronic care delivery problems arises:
- Limited appointment time isn’t enough for patients’ proper education
- Patients don’t know their goals and milestones, and can’t accurately manage their disease
- Physicians are unaware of patients’ health status between appointments and after discharge from the hospital, so they can’t timely suggest scheduling an appointment
The tech trio of healthcare CRM, mobile app, and PGHD can handle this array of issues by becoming the center of patient-physician collaboration.
The CRM system’s role is to track the frequency of appointments and tests, recognize the gaps in the scheduled ones, and, thus, to detect interrupted care cases. For example, if a patient visited his or her physician only once or twice, and then there are no scheduled appointments for a few months (depending on the condition), a system will spot this and inform both the physician and the patient.
Physicians get their notifications from the CRM via email, text, or their medical mobile app, depending on the technical implementation.
The patient-notifying function is enabled via a patient mobile app. Individuals get a message that they haven’t seen their doctor in a while, so it is about time to schedule an appointment. See how it works in this patient app online demo.
PGHD fuels these two tools. Patients measure their vitals, record them in the mobile app, and share them with their physicians. The CRM analyzes both positive and negative trends in the patients’ conditions and sends notifications to both individuals and doctors in case an appointment might be needed to discuss these changes.
Patient engagement: problems and solutions
Unfortunately, current chronic condition management activities don’t fully support patient engagement either. It has to be a constant process, since patients can easily slip into apathy and depression. In the words of WebMD, “it's estimated that up to one-third of people with a serious medical condition have symptoms of depression.”
Reasons can be various – medications' side effects, limited mobility, insufficient social life, exhausting treatment routine, and more.
In the meantime, patients also tend to be careless and reckless; they might underestimate potential risks, which is a straight road to no-shows, mistreated symptoms, acute complications, and exacerbations.
Without the help of technology, there is no way for daily patient engagement.
Support groups? Well, they are not daily, and patients need to live their lives, work, exercise, and spend time with their family. Health specialists’ attention? We've already discussed that continuous calls are unrealistic, and regular nurse visits is an option affordable not to everyone.
The presented CRM-App-PGHD tech equation can handle this one, too.
Thanks to PGHD and integration with an EHR, a CRM can serve for sending personalized messages and content via a patient mobile app and additionally through a website, a patient portal, and emails (click here to understand the process better).
Inside the patient app, there is a vast field to get creative and support a patient. As one of the key components of engagement is a quick result, gamification should work just right. The possible options are achievements, goal-setting, social sharing, badges, promos, accumulating points, and more.
To reveal all the profits of tech-based long-term condition management, let’s follow treatment steps from A to Z.
Tech-based rehabilitation cycle
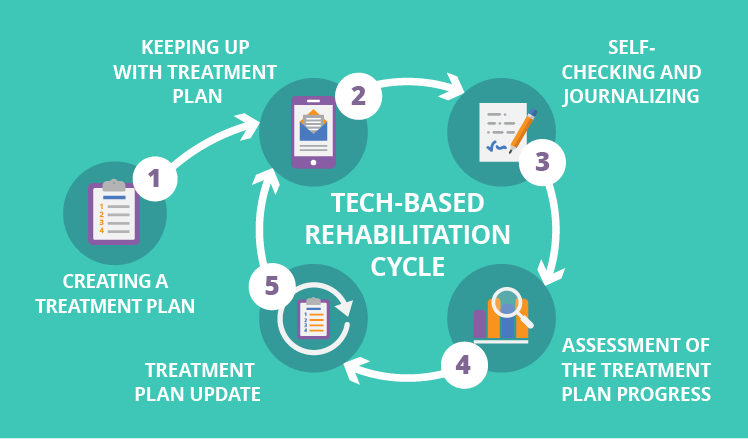
Creating a treatment plan
When a patient is diagnosed with a certain chronic condition, say, diabetes or COPD, the initial treatment plan is created. It consists of weight goals (to gain, lose, or keep), a medication intake scheme, wholesome nutrition choices, blood glucose objectives (for diabetes), target oxygen saturation levels (for COPD), and more.
All primary patient data is recorded in a mobile app via EHR-CRM integration, best during a face-to-face appointment with a physician or during the hospital stay. This allows getting a written patient consent and, what is critical for accurate chronic disease management, to put the correct initial patient data in the app. Moreover, individuals can be sure that this application is official (as it is issued by his or her healthcare provider and set up with a physician), thus, all their information is secure.
Keeping up with the treatment plan
When a patient steps out of the doors of their healthcare organization, he or she is equipped with a mobile application serving as their individual condition management tool. These functional elements below are mostly optional and are embedded according to physicians’ requirements and patients’ needs. Let’s review the examples to understand how such an app works.
Diabetes
To support diabetes management, an application provides patients with personalized content:
- The medication intake scheme with customizable reminders
- Nutrition recommendations (protein food choices, weekly menu plans, macronutrient wheels, and more)
- Therapeutic education (personal hygiene guidelines, early hypoglycemia recognition tips, prescribed exercise program overviews, insulin injection algorithms, etc.)
- Motivation (gamification elements with achievements, badges, goal setting, and social media sharing). For example, care providers can implement rewards for regular tracking of blood glucose with iTunes download points for music, or allow patients to choose their totem animal or fantastic creature and raise it by regularly using the app and recording PGHD.
- Psychosocial support (notifications on diabetes support group gatherings, emergency button for hypoglycemia cases, Q&A chat, and more)
COPD
Patients with COPD can manage it with the help of the following personalized information bits inside their application:
- The medication intake scheme with customizable reminders
- Therapeutic education (breath control techniques, dyspnea management tips, bronchial drainage overview, and more)
- General physical exercises and peripheral muscle training bits of advice (study drills, warm-up videos, meditation podcasts, daily kinesiotherapy sessions, and more)
- Psychosocial support (secure video conversations with a physician, COPD support group meetings announcements, Q&A chat, and others)
- Physiotherapy guide (pre-defined reminders and education materials on inhaling therapy at home, discounts on inpatient procedures such as massage, iontophoresis, balneotherapy)
- Nutritional status support (depending on a patient’s weight goals – lose or gain –particular information is provided, such as how to match anabolic steroids and food, what superfoods are beneficial, how to cook potassium-loaded smoothies, and more)
- Motivation (same as with diabetes, different types of incentives are available: milestones, achievements, progress bonuses, social media sharing, and badges). For instance, care providers can reward patients with bonuses for uninterrupted app entries, which can later be exchanged for gift cards or discounts.
Self-checking and journalizing
We know that chronic disease management works only if individuals stay proactive, so there is no way an app will let patients just sit still and receive instructions. Here, an application serves as a point of the PGHD origin.
To illustrate how a patient copes with achieving objectives and carrying out daily routine, he or she shares their health status information with providers. Most PGHD-sharing functionality is a must in the app, as it allows for the formation of a complete picture of a patient’s condition. Again, we turn to disease-specific examples for better visualization.
PGHD on diabetes
- Subjective (pain, blurry vision, headache, chills, nausea, and more)
- Photos of feet
- Objective (blood glucose level, heart rate, temperature, weight, blood pressure, etc.)
- Insulin and medication intake
- Diet diary (daily hydration and nutrition with carb, protein, and fat consumption)
Patients will have special forms to quickly input their subjective sensations and vitals. If possible, they are also recommended to synchronize other diabetes-related devices (say, insulin pumps, instant glucometers, and CGMs) with the app.
After all daily PGHD is measured and recorded, individuals tap ‘Send’ and contribute to the essential disease management goal – they’re making steps forward to developing a habit of regular health status monitoring. Supporting this habit is very important, so a badge will come in handy. After every sharing activity, a patient might see how his or her mastery bar fills up with more points. Each next level brings a new or upgraded badge.
PGHD on COPD
- Subjective (dyspnea and cough assessment, muscle spasms, discomfort, heartache, and more)
- Medication intake
- Objective (oximetry results, capnography results as an option, temperature, blood pressure, heart rate, weight)
- Diet diary (daily meal and fluid intake with macronutrient breakdown)
For COPD patients, dyspnea and cough assessment can be performed with the help of an application. Care providers implement a particular option at their choice, as different alternatives are possible, from a visual analogue and the Borg point scale to the verbal ‘language of dyspnea’. Cough self-check is also carried out via a visual analogue scale or a cough assessment point scale.
Assessment of the treatment plan progress
Of course, these PGHD flows need to find their way to care providers; otherwise, why should patients bother? Sure, self-management is important, but care consistency exists only if physicians are notified in case the patient's treatment plan performance and significant health status change.
We’ve touched upon this in our ‘systematic care’ section, but now it’s time to dive into details.
Healthcare CRM collects patient-generated data and then puts these raw information pieces into a data analytics module backed by a warehouse. A warehouse is a must here, as we need to store PGHD in its initial form somewhere, and neither EHR nor CRM can support this.
After healthcare data gets into the warehouse, it is processed and analyzed. As there is no perfect patient in the real world, analytics algorithms are created and tuned up to cover most of PGHD quality gaps: interrupted measurements, incomplete data, diverse frequency (whether it is continuous monitoring or a patient manually takes measurements), and systematic errors.
Then patterns are found to highlight both positive and negative trends, as well as correlations in everything a patient reported. Say, when the analytics module detects abnormal (for a particular patient) blood glucose (diabetes) or SpO2 (COPD) trends, it sends this information back to the CRM. From there, the notifications and reminders travel to physicians and patients’ mobile apps, so that they can discuss scheduling an appointment, taking tests, and changing the treatment plan.
And…Voila!
The cycle is completed. The ancient Ouroboros, if you will, has reached its tail. It starts and ends with a face-to-face appointment, which is the best option to:
- install an app and define the initial treatment plan
- assess current treatment progress, discuss PGHD insights, advise tests, and change further patient goals accordingly
Long-term disease management can’t keep up without technology
Without the help of our tech trio, appointments just stay what they always were – disconnected and rare events, unable to shed light on a patient’s real health status.
In the meantime, patients get into a whole world of new routines, habits, procedures, and exercises. Individuals keep this world on their shoulders, but they shouldn’t do this alone. With the technology-based chronic care management model, healthcare providers can embrace a huge part of this weight and lift it up to make patients’ lives easier, healthier, and happier.


